Abstract
Post Transplant Lymphoproliferative Disorder (PTLD) represents one of the most fatal complications following solid organ transplants (SOT). A multicenter analysis in 2010 reported a 3yr overall survival (OS) of 62%. In 2014 a single institutional study reported an improved median OS of 8 years in the rituximab era. Clinical studies have attempted to subdivide post transplant diffuse large B cell lymphomas (PT-DLBCL) into immunophenotypic subgroups with most reviews demonstrating a higher incidence of activated B-cell (ABC) subtype. Because of the rarity of PTLD, insight into disease development and progression is currently limited. We examined the clinical features and outcomes based on immunohistochemical (IHC) analysis in consecutive PTLD pts treated at the University of Colorado over a 25-year period.
Methods: This retrospective analysis focused on 52 adult SOT pts who were treated for PTLD at our institution between Jan 1989 to April 2015.
Results: 52 pts were analyzed. The median age at transplantation was 47.5 years (5-73yrs) and the median time from SOT to PTLD was 52.5 months (2.6 to 251). The most common transplanted organ included liver (46%), kidney (40%), heart (10%), lung (2%) and [kidney pancreas] (2 %). The grafted organ was involved in 10 pts (19%)
Males comprised 67%, 63% were Stage III-IV, 69% were EBV positive, 23% had extranodal involvement, 19% had bone marrow involvement and 21% had CNS involvement. Of the 52 patients, 46 (88 %) had monomorphic histology. Amongst monomorphic PTLD 31 pts (60%) had DLBCL, 6 pts (14%) had Burkitt Lymphoma, 4 pts (9%) had CNS lymphoma, 1 pt (2%) had plasmablastic lymphoma, 1 pt (2%) had NK/T cell lymphoma and 1 pt (2%) had aggressive B cell lymphoma unclassifiable. Of the analyzed pts 85% were CD20 positive, 77 % had elevated LDH and 49% had an International Prognostic Index (IPI) > 1. Thirty Eight pts (73%) were on >1 immunosuppressive agent with a median immunosuppressive treatment duration of 36 months (range 0.25 to 23 yrs).
All pts (100%) diagnosed within 12 months of SOT were EBV positive. Similarly all pts (100%) diagnosed 12 months after were EBV negative.
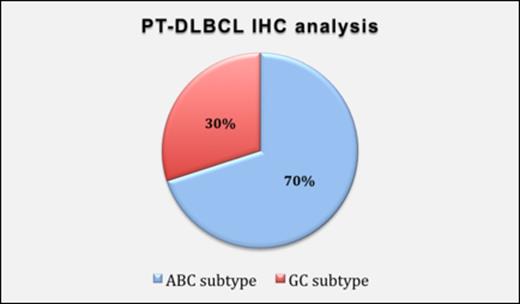
Initial treatments included reduction in immunosuppression in 63% pts, rituximab monotherapy in 28% pts and chemotherapy in 53% pts. 67% of pts received rituximab either alone or in combination with chemotherapy. 48 of 52 pts were assessable for response; 4 pts were lost to follow up. 64% achieved a complete remission after first line therapy while 12% were refractory to front line therapy. 7 of 48 pts (14%) pts relapsed with a median time of 60 months (2yrs-15yrs). IHC staining utilizing the Hans Algorithm was applied on 20/31 pt samples with DLBCL. ABC subtype was identified in 70% (14/20) and GC (germinal center B-cell) subtype in 30% (6/20) samples.
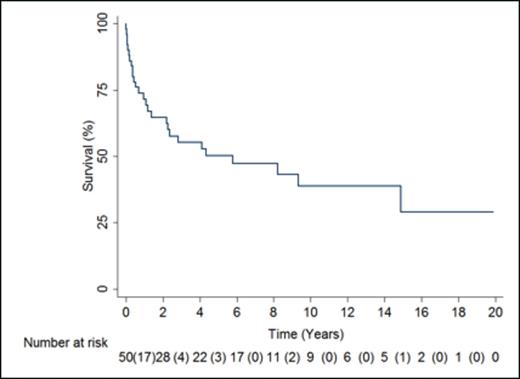
Median overall survival was 69 months (Figure 1).
On univariate analysis CNS disease (HR 2.82, 95% CI 1.25- 6.3, p= 0.01), pts who received chemotherapy (HR 6.65, 95% CI 1.63-27.04, p= 0.008), graft involvement with PTLD (HR 2.63, 95% CI 1.01-6.86, p=0.04) and IPI > 1 (HR: 3.55; 95% CI: 1.47 - 8.57, p= 0.005) were associated with poor survival whereas EBV positivity (HR .25, 95% CI 0.10-0 .64, p= 0.005) was associated with improved survival. Advanced stage (Stage III-IV), high LDH, monomorphic histology, ABC DLBCL subtype, more than 1 immunosuppressive agents and rituximab treatment were not statistically significant parameters for survival.
In multivariate analysis, EBV positivity was predictive of improved survival (p=0.006) while graft organ involvement (p=0.02) and chemotherapy administration (0.013) was associated with poor overall survival.
Conclusion:
In this consecutive series of PTLD after SOT from a single institution over a 25 year period, EBV positivity was associated with improved survival whereas graft organ involvement and chemotherapy was associated with poor outcomes. Similar to previously published data, in PT-DLBCL cases we were not able to demonstrate a definite association between histogenetic phenotype and prognosis. However we found 70% of PT-DLBCL samples to have an ABC subtype (Figure 2). The reason for this increased predilection is not fully understood. ABC subtype is known to have an inferior overall survival compared to GCB DLBCL which could explain the relatively poor outcomes in PT-DLBCL patients. This merits further studies in larger patient cohorts due to potential therapeutic implications.
Pollyea:Ariad: Consultancy; Agios: Consultancy, Membership on an entity's Board of Directors or advisory committees; Celgene: Consultancy, Membership on an entity's Board of Directors or advisory committees, Research Funding; GlycoMimetics: Other: Member of data safety monitoring board; Karyopharm: Consultancy; Pfizer: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.