Abstract
Introduction The International Prognostic Index (IPI) is used to predict survival in patients with diffuse large B-cell lymphoma (DLBCL). The IPI includes five factors: age, stage, LDH, performance status, and extranodal sites. However, studies suggest that certain blood markers not included in the IPI, such as CRP, albumin, absolute lymphocyte count (ALC), and platelet count, predict survival. Recently, an enhanced IPI (NCCN-IPI) was proposed and showed excellent prognostic performance. It uses the same factors as the IPI, but refines the impact of age and LDH and the definition of extranodal disease. Few studies have assessed the prognostic impact of blood markers other than the five factors of the IPI in the context of the NCCN-IPI. Here, we analyzed the prognostic role of simple blood markers in the NCCN-IPI.
Patients and Methods Data from consecutive DLBCL patients diagnosed between January 2004 and June 2014 were retrospectively analyzed. Patients receiving rituximab and anthracycline-based chemotherapy were included in the analysis. Values considered positive were CRP >1 mg/dl, albumin <3.5 g/dl, ALC <1,000/µl, or platelets <100,000/µl. The primary endpoint was overall survival (OS), assessed using the Kaplan-Meier method. The log-rank test and Cox regression analysis were used to assess the prognostic value of each variable.
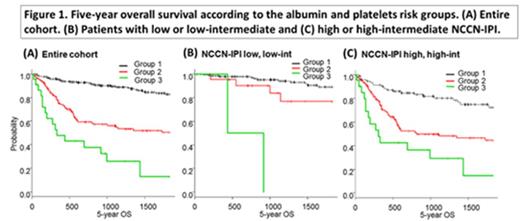
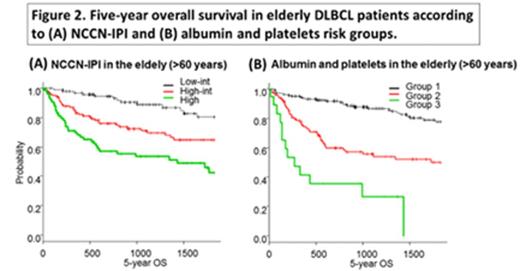
Results A total of 398 patients (median age, 69 years (range, 21-104)) were included. Of these, 124 (31.2%) had an ECOG performance status >1, 221 (55.5%) had advanced stage disease, and 223 (56.1%) had a high or high-intermediate NCCN-IPI score (>3). Pretreatment CRP, albumin, ALC, and platelet count values were positive in 215 (54%), 127 (31.9%), 144 (36.2%), and 31 (7.8%), respectively. The median follow-up was 34.8 months (range, 0.5-134) and the 5-year OS of the entire cohort was 68.8%. Univariate analysis identified CRP [hazard ratio (HR) 3.15; 95% confidence interval (CI) 2.07-4.80, p<0.001), albumin (HR 4.46; 95% CI 2.96-6.7, p<0.001), ALC (HR 2.40; 95% CI 1.62-3.54, p<0.001), platelet count (HR 4.69; 95% CI 2.87-7.67, p<0.001), and NCCN-IPI score >3 (HR 5.05; 95% CI 3.00-8.51, p<0.001) as significant for OS. NCCN-IPI, albumin, and platelet count remained significant in multivariate analysis (NCCN-IPI: HR 3.14; 95% CI 1.77-5.60, p<0.001; albumin: HR 2.41; 95% CI 1.36-4.27, p=0.002; platelets: HR 2.77; 95% CI 1.66-4.61, p<0.001), whereas CRP and ALC did not (CRP: HR 0.91; 95% CI 0.51-1.66, p=0.78; ALC: HR 1.33; 95% CI 0.87-2.03, p=0.18). Based on albumin and platelet count values, patients were divided into three risk groups for OS: group 1 included albumin- and platelet-negative patients (n=247); group 2 included either albumin- or platelet-positive patients (n=128); and group 3 included both albumin- and platelet-positive patients (n=23) (82.6%, 50.2% and 12.9%, respectively; p<0.001) (Figure 1A). The association of these risk groups with OS independently of the NCCN-IPI was evaluated. For patients with low or low-intermediate NCCN-IPI, the 5-year OS for group 1 (n=151), group 2 (n=22), and group 3 (n=2) was 89.2%, 76.8%, and 0%, respectively (p<0.001) (Figure 1B). For patients with high or high-intermediate NCCN-IPI, the 5-year OS for groups 1 (n=96), 2 (n=106), and 3 (n=21) was 72.6%, 44.3%, and 14.6%, respectively (p<0.001) (Figure 1C). Assessment of the prognostic impact of albumin and platelet count in the elderly led to the exclusion of the low risk category (score 0-1) among those older than 60 years (n=291) because of their age score points (>1 points) in the NCCN-IPI; thus, the ability of NCCN-IPI to differentiate risk groups might be diminished in the elderly. For low-intermediate (n=97), high-intermediate (n=118), and high (n=76) NCCN-IPI patients, the 5-year OS for the elderly according to the NCCN-IPI was 80.3%, 64.8% and 42.5%, respectively (p<0.001) (Figure 2A). The combination of albumin and platelet count also predicted survival in the elderly: the 5-year OS for groups 1 (n=169), 2 (n=103), and 3 (n=19) was 77.7%, 50.1%, and 0%, respectively (p< 0.001) (Figure 2B).
Conclusion Despite the improved performance of the NCCN-IPI, albumin and platelet count were independent prognostic factors and predicted survival even in the elderly. Considering albumin and platelets may improve the accuracy of recently established prognostic models. Prospective studies should evaluate the prognostic impact of albumin and platelets.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.