Abstract
Introduction Bone marrow (BM) involvement is an important prognostic factor in DLBCL, which is incorporated into the new prognostic index of NCCN-IPI in rituximab era. Although BM involvement has been evaluated with bone marrow biopsy (BMB), the recent international criteria for staging of non-Hodgkin lymphoma and Hodgkin lymphoma (Lugano criteria) proposed omission of BMB as pre-treatment evaluation in selected cases. However, validity of omission of BMB remains uncertain. Our institute previously reported that the detection of BM clonality using flow cytometry (FCM) or immunoglobulin heavy chain rearrangement (IgR) has prognostic value in DLBCL. Aim of this study is to inspect prognostic value of PET-defined BM involvement combined with clonality of BM.
Patients and Methods We studied consecutive DLBCL patients who were diagnosed in our institute in 2007-2014, received rituximab combined with CHOP-like regimen and undertook pre-treatment staging by FDG-PET/CT, FCM and PCR using BM aspirates. We reviewed the medical records, the staging FDG-PET/CT reports, DICOM images (if available), FCM and IgR reports. BM uptake of FDG was classified as focal or diffuse pattern. Diffuse uptake pattern was not regarded as lymphoma involvement on staging unless lymphoma was proven histologically or cytogenetically. B-cell clonality of BM was defined as positive, either when PCR amplification detected clonal immunoglobulin heavy chain (FR1, FR2, FR3) gene rearrangements with multiplex BIOMED-2 primer sets or when FCM detected κ/λ deviation among B-cell population.
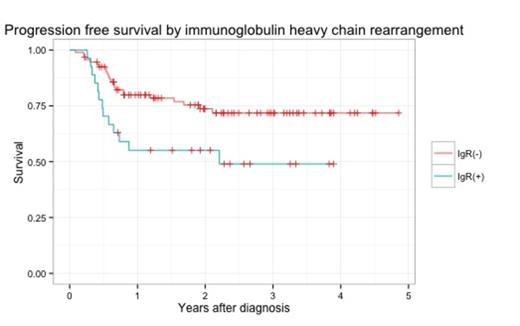
Results One-hundred thirty four patients were identified: median age 69.5 years old (range, 19 - 89), 76 male (57%), LDH above the upper limit in 60(45%), stage ≥ 3 in 69(51%), bulky mass in 10(7.5%), abnormal lymphocytes in BM detected microscopically in 13(9.7%), IPI score were distributed as 0-1 in 46(34%), 2 in 31(23%), 3 in 30(22%) and 4-5 in 27(20%). Thirty patients (22% of the whole cohort) were positive for BM FDG-PET uptakes; the uptake patterns were focal in 23(77%) and diffuse in 7(23%). Follow-up time was median 741 days (range, 31 - 1766). B-cell clonality of BM was found in 20 patients (15%) with FCM and in 27 patients (20%) with IgR. B-cell clonality was more frequently observed in the patients with BM FDG-PET uptake (FCM-based clonality: 37% for positive vs 10% for negative, p-value, 0.002; IgR-based clonality: 38% for positive vs 18% for negative, p-value, 0.034). In addition, IPI score was significantly worse in the BM FDG-PET uptake patients (IPI ≥2: 93% in positive BM FDG-PET uptake vs 58% in negative BM FDG-PET uptake, p-value, < 0.001). Abnormal lymphocytes by BM aspiration did not affect PFS in our cohort significantly (0.14). Patients with BM FDG-PET uptake had more extranodal lesions than patients without BM FDG-PET uptake (mean 0.66 vs 1.6, p-value, < 0.001). In entire cohort, 2-year PFS and 2-year OS were 70% and 83%, respectively. Pretreatment BM FDG-PET uptake had negative impacts on PFS (2-year PFS, 74% for negative vs 53% for positive, p-value, 0.017). Clonality in BM detected with IgR had negative effect on PFS (2-year PFS, 74% for negative vs 55% for positive, p-value, 0.017)(Figure). IPI were also a significant prognostic factor for PFS (2-year PFS, 92% for IPI<2 vs 59% for IPI ≥2, p-value, <0.001). In contrast, clonality using FCM was not a prognostic factor for PFS (2-year PFS, 72% for negative vs 69% for positive, p-value, 0.426). In multivariate analysis for PFS, in which BM FDG-PET focal uptake, clonality using PCR and IPI ≥ 2 (vs <2) were incorporated as covariates, Cox proportional hazard model revealed that clonality using IgR and IPI≥2 (vs <2) into Cox proportional hazard model. As a result, clonality using IgR and IPI≥2 had significant impact on PFS (IgR: HR, 2.27(range, 1.14-4.55, p-value, 0.02); IPI≥2: HR, 7.27 (range, 2.20-24.11, p-value, 0.001). BM FDG-PET focal uptake in BM was not significant possibly because of confounding with IgR and IPI (HR, 1.73(range, 0.81-3.68, p-value, 0.156).
Conclusion Some previous studies showed that BM examination, as well as FDG-PET, had merits for more precise survival prediction. In our study, B-cell clonality of BM is an adverse prognostic factor for PFS that is independent of IPI and the impact of BM FDG-PET status was limited. Although BM clonality was more frequent in the patients whose FDG-PET uptake of BM were focal, BM clonality should be examined combined with FDG-PET.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.