Abstract
Introduction: Idelalisib, a specific small molecule inhibitor of the delta isoform of PI3 kinase (PI3Kd), has recently been FDA approved for the treatment of relapsed CLL. Expression of PI3Kd is predominantly restricted to leukocytes, and inhibition of PI3Kd promotes apoptosis of neoplastic CLL cells. Patients who receive idelalisib often experience toxicities that appear to be immune mediated. In an ongoing phase II study of idelalisib-ofatumumab at DFCI, 16 of 21 patients experienced grade 3 or greater autoimmune toxicities (14 transaminitis, 2 enteritis/colitis and 3 presumed drug-induced pneumonitis).
Methods: To identify potential causes of autoimmunity in patients receiving idelalisib, we used single cell mass cytometry (CyTOF) with a panel of 26 surface membrane and 9 intracellular markers to provide a comprehensive phenotypic and functional analysis of all peripheral blood lymphocytes. Blood samples were obtained at baseline prior to therapy and at onset of autoimmune symptoms, which occurred at a median of 28 days from start of therapy. Results in 5 severely affected patients were compared with 3 patients who did not develop autoimmune toxicities and 15 healthy donors. The second sample from unaffected patients was matched in time to the affected patient samples.
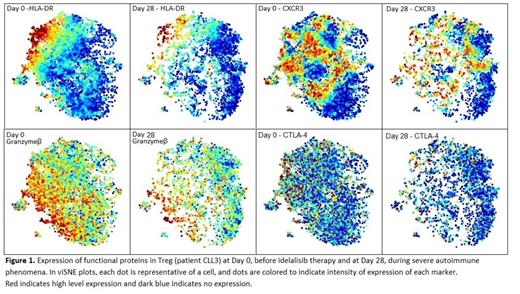
Results: Within CD3 T cells, idelalisib therapy led to an increased percentage of CD4 T cells and decreased percentage of CD8 T cells. Within CD4 T cells, CD25high Foxp3+ regulatory T cells (Treg) were reduced, resulting in a marked increase of the ratio of conventional CD4 T (Tcon)/Treg and increased CD8/Treg ratio. These findings were similar in patients who developed autoimmune toxicities and those who did not. Analysis of effector memory (EM; 45RA- CCR7-), central memory (CM; 45RA- CCR7+), terminal effector (TEMRA; 45RA+ CCR7-) and naive (45RA+ CCR7+) subsets within Treg, Tcon and CD8 T cells was comparable before and after idelalisib therapy and with healthy individual controls. To evaluate the heterogeneity of each population we utilized viSNE, which allows visualization of complex high-dimensional cytometry data on a two-dimensional plot. Treg in patients who developed autoimmune phenomena were compared with Treg from patients who did not. In patients who developed autoimmunity, baseline Treg had higher expression of PD-1 and lower expression of functional markers, such as GITR, Tbet, CXCR3, PDL-1, granzyme-β and TIM-3. In some cases, expression of these functional markers declined further with idelalisib therapy (Figure 1). Cytotoxic T lymphocyte antigen 4 (CTLA4) is constitutively expressed by Treg, and its deficiency has been shown to limit suppressive function of Treg. Inducible co-stimulator (ICOS) also mediates the suppressive functions of CD4 Treg by regulating cell surface expression of CTLA-4. Interestingly, expression of CTLA-4 and ICOS did not change during idelalisib therapy (Figure 1). Susceptibility to apoptosis was monitored by expression of pro-survival Bcl-2 and pro-apoptotic CD95 (FAS). Treg from patients developing autoimmunity expressed lower levels of Bcl-2 and higher levels of CD95 compared to those who did not. Conversely, Treg of non-affected patients retained higher expression of functional markers and became more active, assessed by increased expression of HLA-DR. The use of CyTOF combined with our comprehensive panel allowed us to delineate up to 13 distinct Treg sub-populations among healthy controls. In contrast, CLL patients often lacked such broad Treg heterogeneity. Expression of functional markers by Tcon and CD8 T cells from patients who would develop side effects, were also slightly lower, suggesting that autoimmune toxicities were not due to expansion or activation of CD8 or Tcon effector cells but due to the defect in both number and function of Tregs, which became insufficient to maintain the immune tolerance.
Conclusion: These studies allowed us to identify defects in both Treg number and function, which may be responsible for the autoimmune toxicities in patients receiving idelalisib therapy. Further studies may allow the development of a reliable predictor of these toxicities by evaluation of the Treg markers prior to drug exposure which could be used to guide therapy. Moreover, the identification of idelalisib as a Treg inhibitor suggests that it could be used as an immunomodulatory agent to target the Treg pathway, in patients with solid tumors.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.