Abstract
Background: Bloodstream infection (BSI) is one of serious complications after allogeneic hematopoietic cell transplantation (HCT). Several risk factors have been described in previous reports. They included elderly patients, myeloid malignancies, myeloablative conditioning and HLA mismatch. In recent years, the number of umbilical cord blood used as an alternative donor source is rapidly increasing. The interval between transplant and neutrophil engraftment after umbilical cord blood transplantation (UCBT) is longer than that of other stem cell sources, and bacterial infections are one of the most serious concerns after UCBT. However, studies that focus on the impact of donor source on the incidence of BSI and include sufficient number of UCBT are lacking. In the study, we aimed to analyze the impact of umbilical cord blood on the development of BSI after allogeneic HCT retrospectively.
Patient and Method: We retrospectively studied the patients who received transplant as first allogeneic HCT in Toranomon Hospital between Apr 2003 and Mar 2014. We analyzed the incidence of BSI that occurred within 100 days after transplant. BSI was defined as isolation of a bacterial or fungal pathogen from at least 1 blood culture, with the exception of coagulase-negative staphylococci (CNS) and normal contaminants (Corynebacterium species, Lactobacillus species, Bacillus species and Propionibacterium species), which required 2 separate blood cultures with the same antibiogram, to be considered a true infection. BSI was considered polymicrobial, if 2 or more pathogens were isolated in a single blood culture. The patients whose blood culture was positive within 2 weeks before transplant and the patients whose performance status (PS) were 4 before transplant were excluded.
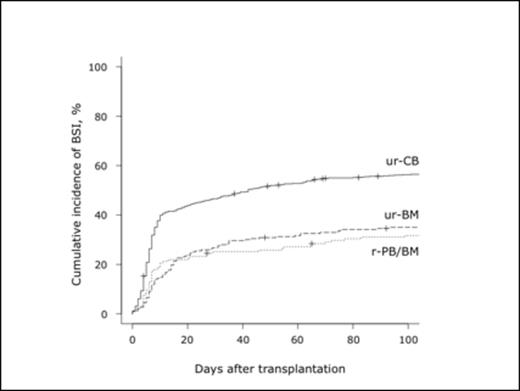
Result: A total of 1032 patients were extracted. Donors were related peripheral blood stem cell and/or bone marrow (r-PB/BM) in 155 patients, unrelated BM (ur-BM) in 243, and unrelated umbilical cord blood (ur-CB) in 634. The median age of recipient was 49 years (range, 16 - 82). Underlying diseases were as follows; AML (n=458), MDS (n=83), CML (n=30), MPN (n=15), MDS/MPN (n=13), ALL/LBL (n=134), CLL (n=3), AUL (n=9), NHL (n=162), HL (n=17), ATL (n=53), MM (n=16), AA (n=35) and others (n=4). The cumulative incidence of BSI was 47.6% (95% confidence interval, 44.5 - 50.6%) at 100 days after allogeneic HCT. The median onset of first BSI was day 7 (range, 0 - 99) after transplant. In 491 patients who developed BSI, a single pathogen was isolated in 409 patients (gram-positive cocci: GPC in 257, gram-negative rod: GNR in 112, gram-positive rod: GPR in 31, fungus in 9). Of the 491 patients with BSI, two pathogens were isolated in 74 patients (two GPCs in 37, one GPC & one GNR in 20, one GPC & one GPR in 13, two GNRs in 3, one GNR & one GPR in 1) and three pathogens were isolated in 8 patients (three GPCs in 5, two GPCs & one GNR in 1, two GPCs & one GPR in 1, one GPC & two GNRs in 1). Of the 581 isolates, GPCs accounted for 66%. The most frequent isolates in GPCs and GNRs were Staphylococcus epidermidis (34% in GPCs) and Pseudomonas aeruginosa (33% in GNRs), respectively. The cumulative incidence of BSI after transplants from r-PB/BM, ur-BM, ur-CB was 31.7%, 35.0%, 56.3%, respectively (p<0.01). In univariate analysis, age (>49 vs. ≤49, p<0.01), PS (2-3 vs. 0-1, p<0.01), hematologic disease (myeloid vs. others, p=0.01), disease status (not in CR vs. in CR, p<0.01), conditioning regimen (MAC vs. RIC, p<0.01), donor source (ur-CB vs. rPB/BM and ur-BM, p<0.01) had impact on the cumulative incidence of BSI. In multivariate analysis, ur-CB was identified as the most significant risk factor for the development of BSI (hazard ratio 1.60, 95% confidence interval 1.34 - 1.92, p=0.00000017).
Conclusion: The study included 634 UCBT and it allowed us to clarify the impact of umbilical cord blood on the development of BSI. We concluded that umbilical cord blood was the most significant risk factor for BSI after allogeneic HCT. BSI should be recognized as a serious complication that emerges in more than a half of recipients in the early phase after UCBT.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.