Abstract
Background
Natural Killer (NK) cells have been widely studied due to their non-major histocompatibility complex (MHC)-restricted cytotoxicity towards transformed or virally infected target cells. In the setting of hematopoietic stem cell transplantation (HSCT), donor NK cells may be "alloreactive" as their killer immunoglobuline-like receptors (KIRs) do not recognize their ligands on recipient human leukocyte antigen (HLA) class I molecules (i.e. KIR-ligands), leading to NK activation. NK alloreactivity can often occur in haploidentical HSCT (Haplo-HSCT), by means of KIR/KIR-L mismatch in graft versus host (GvH) direction, contributing to graft-versus leukemia (GvL) effect, clearing residual leukemic blasts. In the last decade, several studies have shown that NK cells alloreactivity plays a role in T-depleted Haplo-HSCT leading to higher disease free survival rates for patients transplanted from NK-alloreactive donors; recent studies have also shown that donors having KIR B haplotypes (characterized by the presence of more activating KIR) or expressing KIR2DS1 correlated with a better clinical outcome of transplantation. Thus, these NK cell features might be positively considered in the donor selection strategy.
Materials and Methods:
We analyzed NK-alloreactivity in the setting of unmanipulated Haplo-HSCT with post-transplant cyclophosphamide for patients affected by acute myeloid leukemia or myelodisplastic syndromes. 101 consecutive patients transplanted from September, 2010 to October, 2014 were enrolled, with the big majority of donors and patients studied for HLA-genotype and KIR.
Results:
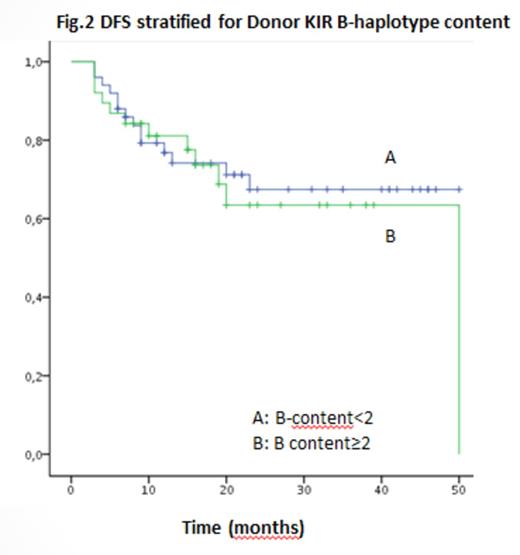
Disease status at HSCT was the most relevant factor affecting outcome (p <0.0001), with 3 y 78% overall survival (OS) and 76% disease free survival (DFS) rates for "early" patients (CR1+CR2, n=61) versus 33% OS and 28% DFS rates for "advanced" patients (CR3 or active disease, n=40). Nor NK-alloreactivity nor the presence of donor KIR-B haplotype nor the presence of donor KIR2DS1 seemed to play a role in preventing leukemia relapse. NK alloreactive patients had DFS rate similar to non-NK alloreactive group (62% vs 59%, p 0.47) with a better, still non-significant trend in OS (72% vs 60%, p 0.14) for NK-alloreactive patients. Similarly, Haplo-HSCT from donors with KIR-B haplotype (with B-content score>=2) or who had KIR2DS1 was not associated with better outcome (p 0.67 and p 0.89, respectively). We observed an high expression of CD56 and inhibitory receptors such as NKG2A on surface of NK cells in post-HSCT samples, suggesting that NK-cell function could be inhibited in unmanipulated haploidentical setting.
Conclusions
NK alloreactivity seems not to play a role in preventing leukemia relapse in unmanipulated haploidentical transplantation with post-transplantation. The different immunosuppressive approach of this Haplo-HSCT setting compared to T-depleted Haplo-HSCT, with concomitant use of cyclosporine from early transplant days, which has been shown to interact and possibly inhibit NK cells in vivo, and post transplant cyclophosphamide effects, selectively killing activated T-cell and inducing long-term tolerance, could affect NK efficacy. Further studies are needed to better understand the complexity of this intriguing issue, leading to a more complete definition of NK cell functions in this Haplo-HSCT setting.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.