Abstract
INTRODUCTION
Nephrotic Syndrome, one of the most common forms of glomerular disease, is characterized by massive proteinuria with structural and functional injury of specialized glomerular cells called podocytes.We and others have shown that thrombin generation is enhanced in nephrotic syndrome. Recent in vitro studies have demonstrated that exposure to high concentrations of thrombin can injure podocytes, suggesting that thrombin may exacerbate glomerular injury. However, the molecular mechanisms by which thrombin induces podocyte injury are not yet known. Thrombin activates platelets, leukocytes, and other cells via the protease activated receptor (PAR) system. Thus, we hypothesized that thrombin exacerbates glomerular injury by enhancing podocyte apoptosis in a PAR-dependent manner.
METHODS
Experiments were performed with differentiated, conditionally immortalized human podocytes. After 36 hours of thrombin (20nM) exposure podocyte apoptosis was determined by TUNEL assay. Specific PAR antibodies and activating peptides were utilized to determine which PARs mediate thrombin-induced podocyte apoptosis. Specific PAR antibodies (ab) included hPAR1ab (ATAP2), hPAR2 ab (SAM11), hPAR3 ab (8E8), hPAR4 ab (H-120). Activation peptides (AP) included PAR1 AP (TFFLRNPNDKNH2), PAR2 AP (SLIGRLNH2); PAR3 AP (TFRGAPOH); PAR4 AP (AYPGKFNH2) and a control peptide (FSLLRNNH2). Phalloidin assays were used to evaluate structural changes in the actin-cytoskeleton as a marker of podocyte stress. Proximity ligation assays (PLAs) allow detection of protein-protein interactions at the molecular level. PLAs were performed on podocytes grown in an 8-well chamber slide system. PLA was carried out using the DUOLinkTM kit (Sigma-Aldrich) according to the manufacturer's instructions and as described previously. Oligonucleotide-conjugated secondary antibodies against mouse and rabbit primary antibodies were used and protein-protein associations were detected by microscopy as bright red dots. One-Way ANOVA and t-tests were used to determine statistical significance (SigmaPlotTM).
RESULTS
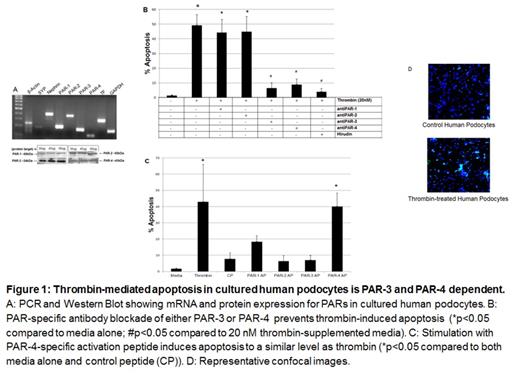
Thrombin exposure induced a significant increase in apoptosis of human podocytes from 1.8% to 42.87% (p <0.05). Blockade of PAR-3 or PAR-4 resulted in a significant decrease in apoptosis [9.2% with hPAR-3 ab and 11.7% with hPAR-4ab] (p <0.05). Inhibition of thrombin enzymatic activity with hirudin, a direct thrombin inhibitor, also resulted in a decrease in apoptosis to 2.1% (p <0.05). In comparison to a control peptide, PAR-4 activation peptide significantly increased apoptosis from 1.7% to 40.1% (p <0.05), while PAR-3 activation peptide did not. Analogous results were seen with the phalloidin assay. Thrombin caused actin cytoskeletal changes, while PAR-3 and PAR-4 blockade ameliorated these changes. In addition, only activation with PAR-4 activating peptide resulted in loss of actin stress fibers. These findings suggest that, in human podocytes, thrombin signaling is mediated via PAR-4, in a PAR-3-dependent manner.
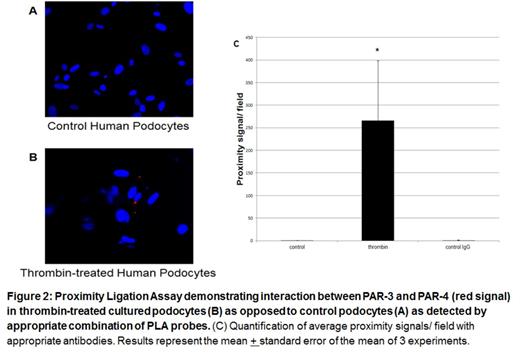
Thus to directly assess this hypothesis, we performed proximity ligation assays with PAR-3/PAR-4 antibodies in the presence and absence of thrombin which revealed the presence of PAR-3/PAR-4 interactions in thrombin exposed podocytes, but not in control podocytes. The quantification of the in situ PLA signals per cell was performed with a BZ900 microscope and software (Keyence, Osaka, Japan) equipped with automated 'dynamic cell count" feature (p =0.03).
CONCLUSIONS
Thrombin-induced injury is mediated in a PAR-dependent fashion in human podocytes. Specifically, in this in vitro model, thrombin-induced apoptosis appears to be mediated in a PAR-3/-4 dependent manner. Furthermore, these data suggest that thrombin induced podocyte injury may be mediated in a manner dependent on interactions between PAR-3 and -4. This is a novel finding, as PAR-3/-4 interactions are known to mediate mouse platelet signaling, but have not been previously described in human cells. Collectively, our findings suggest that interrupting thrombin-mediated podocyte injury may offer a novel therapeutic approach to reduce podocyte injury during nephrotic syndrome.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.