Abstract
Background: Adult T-cell acute lymphoblastic leukemia / lymphoma (T-ALL) is a rare and aggressive hematological malignancy. Unlike B-cell ALL, apart from age and presenting WBC, additional prognostic factors remain largely unknown. Additionally, the prognostic impact of a monosomal karyotype, which has a negative impact on survival in myeloid neoplasms, remains to be determined in T-ALL (Kenderian et al, BCJ 2013)
Aim: To study predictors of survival including the role of a monosomal karyotype in T-ALL.
Methods: After due IRB approval, adults diagnosed with T-ALL from 1990-2014 at Mayo Clinic Rochester were identified. All clinical and pathologic data including FISH studies and cytogenetics were retrospectively reviewed. Chi-square test was used to compare variables. Survival was estimated and compared using the Kaplan-Meier Method and log-rank test. Univariate and multivariate analysis was performed using the Cox regression model.
Results: Between 1990 and 2014, a total of 92 consecutive patients (pts) with T-ALL were identified, 41 had acute lymphoblastic lymphoma (LBL), and 51 (55%) acute lymphoblastic leukemia (ALL). Median age at diagnosis was 33 years (range; 18-88 years) with 72%males. Median follow up of our cohort was 25 months (range; 0.9-260 months) during which time 42 deaths (45%) were documented.
A. Baseline characteristics: Fifty six (67%) had constitutional symptoms, and 63 (77%) had lymphadenopathy at diagnosis. Mediastinal mass was identified in 49 (55%) pts with palpable splenomegaly in 16 (20%) pts. Fifty one (58%) pts had extranodal disease, and 17 (19%) pts had CNS involvement. Pleural and pericardial effusion were evident in 16 (19%), and 6 (7%) pts, respectively. Median laboratory values included; LDH 288 U/L (115-6590), hemoglobin (Hb) 12.8 g/dl (4.5-18.2), WBC 8.65 x109 (1.4-406), platelets 169 x109 (8-485), bone marrow blasts 29% (0-99).
B. Treatments: Induction therapies were variable and included; 11 (12%) CHOP like regimens, 7 (8%) modified NHL regimens (Asparginase+CHOP), 54 (58%) ALL like regimens (CALGB 9111, E2993, or HyperCVAD), 13 (14%) Pediatric regimens (ALL 10403, CCG 1961, BFM, Augmented BFM, GRAALL 2003, or Hoelzer regimen), with 7 (8%) patients' receiving palliative care only. Seventy-one (77%) pts achieved complete remission (CR1) during induction therapy while eight pts had refractory disease (8%). Thirty-three (35%) pts underwent stem cell transplant; 7 (21%) autologous and 26 (79%) allogeneic. Forty one (44%) pts had disease relapse and median time to relapse was 10.8 months (range; 8.2-16 months)
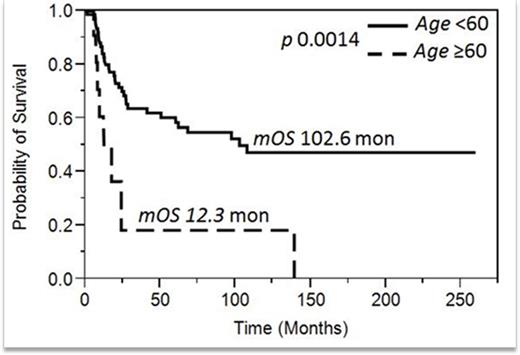
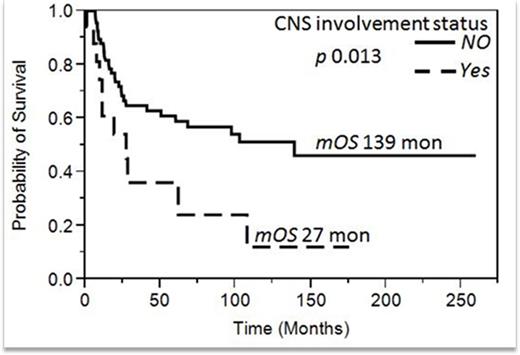
C. Predictors of survival: In univariate analysis, that included age > 60 years, leukocyte count Hb, Plt, Blast percentage, mediastinal mass, LDH and CNS involvement, only age >60 and CNS involvement were predictors of inferior survival and both retained significance in the multivariable analysis with HR 3.9 (CI 1.5 - 9; p=0.0055) and 2.8 (1.3 - 5.7; p =0.0085), respectively (Figure 1 and 2). In this cohort age >60 was a better stratification that the conventionally used age above 40 (p = 0.1). Among 56 pts with evaluable cytogenetics data, 7 (13%) pts had MK which did not have an impact on survival with HR 1.9 (CI 0.4-5.6; p=0.33).
Conclusion: In this large cohort of adult T-ALL patients, we observed that age >60 years and CNS involvement were independent predictors of inferior survival. MK was infrequent, but unlike in myeloid neoplasms, does not seem to impact overall survival.
Al-Kali:Celgene: Research Funding. Thompson:Kite Pharma: Research Funding. Witzig:Novartis: Research Funding; Celgene: Research Funding; Amgen: Honoraria; Spectrum: Research Funding; Valeant Pharma: Equity Ownership.
Author notes
Asterisk with author names denotes non-ASH members.