Abstract
Introduction. Multiple myeloma (MM) represents a population with an increased risk of developing infection up to 10-fold if compared with controls. Moreover, patients treated with new-drugs are at higher risk of infections compared with those treated previously (Blimark C. et al. Haematologica 2015). Grade 3-4 non-hematological toxicity, particularly cardiac and infection complications, are associated with shorter OS in patients with MM (Bringhen S. et al. Haematologica 2013) whereas thrombosis did not. Anyway, guidelines to prevent thrombosis are available but there are not as regard infections although they would be advisable since infections still represent one of leading non-hematological adverse event in any protocols.
Methods. Newly diagnosed MM patients included in 2 prospective trials (VMP vs VMPT, Palumbo et al. JCO 2014; MPR vs MEL-200, Palumbo et al. NEJM 2014) were studied with the aim to assess probability, type, severity, timing and factors predictive of grade 3-5 infectious complications (according to CTCAE version 4.03) occurred during the first years of treatment with these bortezomib or lenalidomide combinations. Patients who underwent autologous transplantation were censored at the time of transplant. Infections were classified according to Immunocompromised Host Society criteria (J Infect Dis, 1990). All patients received thrimethoprim-sulphamethoxazole prophylaxis and patients treated with bortezomib received anti-viral prophylaxis, yet.
Results. Four-hundred and seventy-six patients were analyzed. Median age was 66 years (range 36-85). Karnofsky performance status (KPS) was < 70 in 115 patients (24%), 106 (22%) had IgA heavy chain myeloma, 106 (22%) had ISS stage 3, 14 (3%) had renal insufficiency and 103/343 evaluated (30%) had unfavorable cytogenetic. Bortezomib combinations was administered to 257 patients (54%; 152 VMP, 105 VMPT) whilst 219 received lenalidomide combinations as induction-consolidation therapy (46%; 132 Rd, 87 MPR).
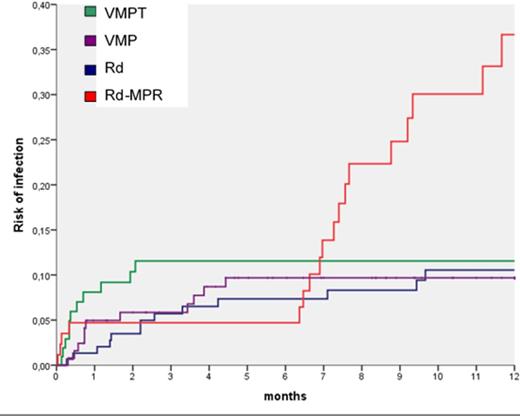
One-hundred and fifty-eight febrile episodes (33.2%) were identified within the study population. Grade (G) 3-5 infections occurred in 53 patients (11%; G3=45, G4=7, G5=2). Out of these latter, 29 (55%) infections were clinically documented (pneumonia=22, soft tissue=5, gastrointestinal=2), 8 (15%) were microbiologically document (bacterial=7, viral=1) and 17(30%) were FUO (febrile neutropenia=11, sepsis=6). Pneumonia was the prevalent type of infection during treatment with Rd, VMP or VMPT whilst most febrile neutropenia or sepsis occurred during MPR treatment. Overall, probability of grade 3-5 infection was 13% at 12 months. However, the probability of infection reaching a plateau at 10-11% at 4 months in patients treated with Rd, VMP or VMPT whereas there was a second peak of infection at 35% probability at 12 months in patients treated with Rd followed by MPR consolidation (Fig. 1). Stepwise Cox regression analysis showed that KPS<70 (HR: 2.4; CI95%: 1.3-4.2; p=0.003), ISS stage 3 (HR: 2.1; CI95%: 1.2-3.7; p=0.013) and MPR regimen (HR: 2.1; CI95%: 1.2-3.8; p=0.017) were independently associated with increased risk of infection whereas age> 65 years, male sex, IgA myeloma type, renal failure, presence of plasmocytoma, unfavorable cytogenetic, bone marrow plasma cells > 60% and new agent used in induction (bortezomib or lenalidomide) were not. No significant difference in OS was found between patients who have had or not an infection (59 vs 71 months; p=0.333).
Conclusions. This study suggests that, in patients with newly diagnosed MM treated with bortezomib or lenalidomide combinations, infections are a frequent cause of morbidity but not of mortality. Infections, mainly pneumonia, usually occurred in the first 4 months; however, when MPR was used as consolidation after Rd, the risk of unusual and severe infections continues all time long. Besides anti-PJ and anti-VZV prophylaxis, patients with poor KPS, with high tumor burden and who underwent MPR regimen, should receive antibiotic prophylaxis and they may be the ideal candidates to be included in a prospective, randomized study regarding antibiotic prophylaxis to prevent severe bacterial infections.
Offidani:Celgene, Janssen: Honoraria. Off Label Use: Lenalidomide. Corvatta:Celgene, Janssen: Honoraria. Bringhen:Onyx: Consultancy; Janssen-Cilag, Celgene, Novartis: Honoraria; Merck Sharp & Dohme: Membership on an entity's Board of Directors or advisory committees. Gentili:Celgene, Janssen: Honoraria. Gay:Celgene, Janssen: Honoraria. Boccadoro:Celgene, Janssen: Consultancy, Honoraria. Palumbo:Celgene, Janssen: Consultancy, Honoraria, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.