Abstract
Background/Aim: Despite recent advances in the management of ALL, alloHSCT remains standard of care for younger adults with high-risk features. The optimum conditioning regimen for adults is not yet established. There is evidence for usage of Etoposide or higher-dose TBI in advanced disease transplants for ALL in a mixture of adult and paediatric patients (Marks et al, Biol BMT, 2006) We undertook a retrospective analysis of adult ALL patients who underwent allogeneic stem cell transplantation at our centre to find out factors influencing outcome and early treatment related complications. We also compared between Cyclophosphosphamide and Total Body Irradiation (Cy/TBI) and Etoposide and Total Body Irradiation (Etop/TBI).
Method: Patients were identified from a transplant database search from January 2000 to May 2015 at the Alfred Hospital Melbourne, Australia. Decision to transplant the patients were based on high risk factors such as adverse cytogenetics (Ph+, MLL, complex karyotype), high presenting WBC count, delayed blast clearance with induction treatment and relapsed and refractory disease. Patients were compared based on transplant conditioning, disease factors and analysed for disease outcomes and complications. We also stratified the patients based on EBMT risk score and investigated the applicability of the score to predict outcome. High EBMT score was defined as >3.
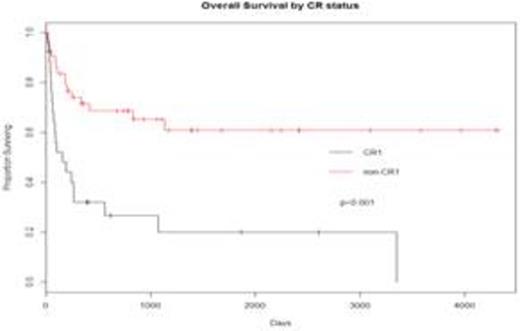
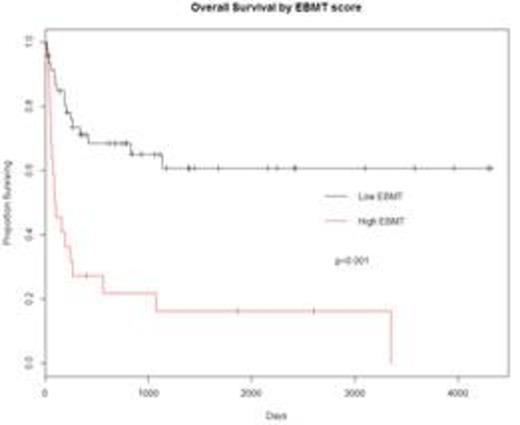
Results: 69 patients identified (34 Cy/TBI, 35 Etop/TBI) with median age of 33 years (range 17 - 59 years). Age was comparable for each group (Cy/TBI 35 years, Etop/TBI 31 years, p=0.84). 52 patients were males. The diagnoses were B ALL(49),T ALL(15), Bilineage Leukemia(1) and ambiguous lineage leukemia(1). 27 sibling and 42 non-sibling transplants, similar proportion for each conditioning (p=0.14). T-cell depletion with antithymocytic globulin used in 43 cases (all non-sibling and 1 sibling). High EBMT scores seen in 22 patients, with significantly higher numbers in Cy/TBI group (47% vs. 17%, p=0.01). 43 transplants done in CR1, 8 in CR2 and 18 in active-disease. There were significantly higher non-CR transplants in the Cy/TBI group (55% vs. 20%,p=0.003). Stem cell source was bone marrow in 10 patients (6 in CyTBI, 4 in Etop/TBI, p=0.5). 18 patients developed grade 3-4 acute GVHD and 13 of them were from Etop/TBI group (p=0.09). 28 patients developed extensive chronic GVHD and 20 of them received Etop/TBI conditioning(p=0.006). TRM was similar in both groups (38% vs. 31%, p=0.62). TRM was lower in patients transplanted in CR1 versus non-CR1 (25% vs. 50%, p=0.04). Median overall survival (OS) was 263 days in the Cy/TBI group versus not reached in the Etop/TBI group (p=0.08). In patients transplanted in CR1, OS was similar (NR, p=0.59) with a predicted 3-year OS of 77% and 62% in Cy/TBI and Etop/TBI groups respectively. OS was superior in CR1 transplants compared to the rest (NR vs 174 days, p<0.001). There was no difference in outcome between sibling and matched unrelated transplants (p=0.12). Patients with a high EBMT score had inferior OS (99 days vs NR, p<0.001) and TRM (63% vs 21%, p<0.001).
Discussion: Outcomes for allogeneic stem cell transplant are similar for Cy/TBI and Etop/TBI for transplants performed in first remission, with equivalent outcomes for sibling and unrelated donor transplants. The rates of chronic graft vs. host disease are higher in Etop/TBI conditioned transplants. The EBMT score was highly predictive of outcome in ALL transplants, with high transplant related and disease related mortality. While long-term survivors are seen with Etop/TBI conditioning in non-CR1 transplants, the outcome in this patient group are very poor, highlighting the need for better prediction of relapse risk to aid appropriate patient selection for allografts in CR1.
Wei:Amgen: Honoraria, Membership on an entity's Board of Directors or advisory committees; Celgene: Membership on an entity's Board of Directors or advisory committees, Research Funding; Novartis: Membership on an entity's Board of Directors or advisory committees; Servier: Membership on an entity's Board of Directors or advisory committees, Research Funding; Abbvie: Membership on an entity's Board of Directors or advisory committees, Research Funding; Agios: Membership on an entity's Board of Directors or advisory committees; Astra Zeneca: Membership on an entity's Board of Directors or advisory committees; Bayer: Membership on an entity's Board of Directors or advisory committees; Roche: Membership on an entity's Board of Directors or advisory committees.
Author notes
Asterisk with author names denotes non-ASH members.