Abstract
Background: Survival of patients with cardiac AL amyloidosis remains poor due to high mortality in the first 6-12 months. Rapidly effective regimes such as CyBorD are unable to overcome poor prognosis in very advanced AL amyloidosis (Venner et al and Palladini et al Leukemia 2014). The median survival of moderately advanced AL is ~60% at 2 years with CyBorD (Palladini et al Blood 2015). Last year, we reported a small series suggesting that oral doxycycline improves survival in cardiac AL amyloidosis (Wechalekar et al ASH abstract 2014) based on the possible cardio-protective effect of doxycycline on the heart from toxic amyloidogenic light chains. We now report a larger cohort confirming those findings.
Methods: All patients with cardiac AL amyloidosis treated at the Royal Free Amyloidosis Treatment Centre, London, received oral doxycycline as adjuvant to standard chemotherapy. Doxycyline was given orally 100 mg twice daily until completion of treatment and continued as long as tolerated without unacceptable toxicity or patient preference. A cohort of matched control patient (approximately two controls for each patient) (matched based on cardiac disease stage, absolute NT-proBNP level, age and presenting dFLC) was randomly selected from the cohort of 1000 patients treated in the prospective ALChemy trial. The primary outcome measure was overall survival, haematological response and cardiac response. Organ involvement, haematological/organ responses were defined as per the 2010 amyloidosis consensus criteria.
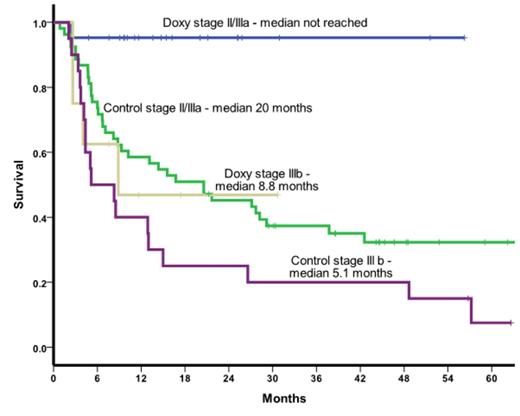
Patients and results: A total of 30 patients treated with doxycycline and 73 mathced controls were identified. The median age was 65 yrs (range 47-87 yrs), all patients had cardiac involvement with 6 having Mayo stage II (2 doxycycline and 4 controls), remainder with Mayo stage III disease (including 28 with Mayo stage IIIb disease). The median NT-proBNP was 4728 pMol/L (range 559-37889), high sensitivity troponin 0.1 mcg/L (range 0.032-0.95), eGFR 63 ml/min (range 15-100) and dFLC 505 mg/L (range 54-3428). There was no significant difference at baseline between the treated and control groups in terms of length of follow up, supine systolic BP, LV wall thickness, ejection fraction, NT-proBNP, hs-TNT, eGFR, proteinuria or dFLC. 72% had a velcade based regime, 23% had a thalidomide based protocol and 5% melphalan based regime. 23% in the doxycycline and 16% in the control group switched treatment due to lack of deep clonal response. The median duration on doxycycline was 6 months (range 1-24 months). Three patients had to discontinue doxycycline early (2 months each) due to photosensitive rash in 2 and nausea in one patient. Overall 33% achieved a complete haematological response (CR), 9 % VGPR and 29% PR. In the doxycycline group 56% achieved a CR, 10% had a VGPR, 30% PR compared to 35% CR,.8% VGPR, 37% PR in the control group. The median follow up of the whole cohort is 13 months and there were a total of 58 deaths. 72% of the control patients have died compared to 16% of the doxycycline treated group (at 2.3 months). The median overall survival was 13 months in the control group and not reached in the doxycycline group. The 12 and 24 month survival in the doxycycline treated group was 82% and 82%, respectively compared to 53% and 40% in the control group (log rank p<0.0001). The survival advantage was marked in stage IIIa patients but there was no impact of doxycycline in the stage IIIb patients. On an intent to treat basis, 60% of the doxycycline group and 18% of the control group achieved cardiac responses by NT-proBNP criteria (chi square p<0.0001).
Conclusions: Treatment with doxycycline in combination with chemotherapy significantly improves the overall survival in patients with advanced cardiac stage IIIa AL amyloidosis but not in those with very advanced stage IIIb disease. There was a significantly a higher CR/VGPR rate compared to controls which translated into significantly greater number of cardiac responses. This larger study confirms the previous preliminary results of using adjuvant doxycycline in AL amyloidosis and strongly support the rationale to proceed with a randomised trial.
Wechalekar:Celgene: Honoraria; Takeda: Honoraria; Amgen: Research Funding. Off Label Use: Doxycycline for AL amyloidosis.
Author notes
Asterisk with author names denotes non-ASH members.