Abstract
Introduction
Heterozygous RTEL1 mutations have recently been described in familial pulmonary fibrosis (PF) but are not known to be associated with cytopenias or bone marrow failure (BMF), in contrast to heterozygous mutations in other telomere maintenance genes TERT, TERC and TINF2. Constitutional BMF syndromes typically present with less severe pancytopenia and it is often unclear if they have hypocellular MDS (hypoMDS) or non-severe AA (NSAA) morphologically.
Methods
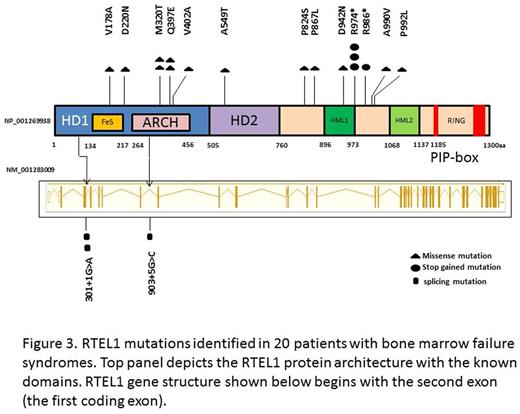
We screened 284 patients with idiopathic AA or uncharacterised BMF and 172 patients with MDS or acute myeloid leukemia (AML) for TL and RTEL1 variants, and for the other currently known telomere gene complex (TGC) mutations, after excluding patients with Fanconi anemia, DBA or other known inherited BMF syndrome. TL was measured using a monochrome multiplex quantitative PCR method on peripheral blood mononuclear cells. Illumina Nextera-amplicon sequencing was used to screen exons of the DC genes (DKC1, TERC, TERT, RTEL1, CTC1, NHP10, NOP2, USB1, WRAP53, TINF2, PARN and ACD) by MiSeq platform. Constitutional DNA was also analysed in 10 patients (skin 9, buccal swab 1) with RTEL1 variants. A targeted gene panel of 24 genes of an Illumina Tru-Seq Custom Amplicon workflow and platform was used to identify genes frequently mutated in MDS/AML. Impact of mutations was predicted based on 3D structure information from comparative modelling for the helicase domain, comprising the HD1 and HD2 subdomains, a Fe-S cluster and an ARCH domain, and for two harmonin-like (HML) domains and a RING finger domain, located in the C-terminal regulatory region of RTEL1.
Results
Heterozygous RTEL1 variants were identified in 20 (4.4%) patients. RTEL1 variant allele frequency (VAF) was 45-70% consistent with heterozygous inheritance in all cases. TL was short in 18 (90%) patients, being < 1st centile in 15 and <10th centile in 3. 2 patients had normal TL, <20th centile and >50th centile, respectively. Median age was 35 years (range 18-73). 15/20 (75%) had a hypocellular BM (7 hypoMDS, 5 non-severe AA, 3 ICUS), and 1 each with RAEB1, RAEB2, CMML1, AML and isolated macrocytosis. 3 patients had abnormal karyotype: +8 (hypoMDS), -Y,+1,del(1) (hypoMDS), del7q (RAEB1). 2 other patients with hypoMDS had somatic mutations: U2AF1 (30% VAF) with ASXL1 (27% VAF); U2AF1 (43% VAF). Lung abnormalities were early PF (1), interstitial lung disease (1), and abnormal lung function with reduced TLCO (1) and an obstructive picture (1). Liver fibrosis with portal hypertension and varices and reticulate skin pigmentation were present in the patient with ILD, 2 patients had dystrophic nails, and 1 unexplained mild hepato-splenomegaly. 2 patients had familial MDS, 5 had a family history of cancers affecting first-degree relatives, and 2 had skeletal and cartilage anomalies, associated with learning difficulties in 1 patient. 8/15 patients with hypocellular BM required no treatment (5 hypoMDS and 3 NSAA), one hypoMDS had CR with ciclosporin and another underwent successful unrelated donor stem cell transplant; for NSAA, 2 received ATG with CSA, with PR followed by relapse in one, the other was lost to follow up, and 1 was androgen responsive. 16/20 (80%) patients are alive; 3 patients with RAEB or AML died of progressive disease and 1 patient with ICUS and severe constitutional features died from lymphoma 10 years after presentation.
Mutations were spread throughout the entire RTEL1 sequence (summarised in Figure). 3D structure analysis predicted the missense RTEL1 mutations would result in disturbance of the FeS cluster and/or interfere with DNA binding, destabilisation of the HD1, HD2 or the ARCH sub-domains of the helicase domain, or destabilisation of inter-domain interactions. One HML1 mutation occurred in a loop opposite the putative ligand binding site and the rest in the variable regions outside the conserved domains. RTEL1 variants were associated with TERT mutations in 4 patients, of which 3 were known pathogenetic and 1 novel TERT mutation with low telomerase activity on TRAP assay confirming its pathogenetic nature.
Conclusions
We show for the first time that heterozygous RTEL1 mutations occur in 4.4% of patients, most commonly in young patients with a hypocellular BM, and often a family history of BMF/malignancy, and less often with high risk MDS/AML. Abnormal clinical features were present in a third of patients, some similar to but others distinct from dyskeratosis congenita.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.