Abstract
Introduction: Diffuse large B-cell lymphoma (DLBCL) is the largest subtype of lymphoma, but consists of heterogeneous groups with different prognosis. Many studies conducted to determine prognosis factors of DLBCL. Recently, several studies have been reported that the elderly Epstein-Barr virus (EBV)-positive DLBCL patients showed worse prognosis than the elderly EBV-negative DLBCL. (Oyama T et al. Clin Cancer Res 2007;13:5024-5032). On the other hand, other studies reported that EBV-positivity is not a prognosis factor in young-adult DLBCL patients (Hong JY et al. Annals of Oncology 2015;26:548-555, Nicolae A et al. BLOOD 2015;126:863-872). In the present study, retrospective analyses were carried out for patients with DLBCL diagnosed between 1990 and 2007 to analyze the clinical and prognostic significance of EBV.
Patients: Those who met the following criteria were included in the study: (i) pathology confirmed de novo DLBCL, according to the WHO classification; (ii) adequate amount and quality of paraffin-embedded biopsy specimens or unstained slides for EBV-encoded RNA in situ hybridization.
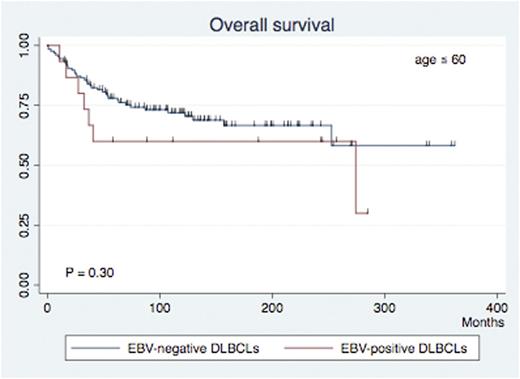
Statistical methods: Intergroup comparisons were carried out with Fisher's exact test for categorical variables and the Mann-Whitney test for age. For survival analysis, we carried out Kaplan-Meier and multivariate proportional hazard (Cox) analyses. Statistical analyses were carried out using the software Stata SE version 14.0.
Results: A total of 456 patients were included. The median follow up duration of survivor was 100 months (range, 1.9-363). There were 236 male (51.75%) and 220 female patients (48.25%) with a median age of 67 (range, 22-94) years. 246 patients (54.0%) were in advanced (III/IV) stage, 134 (29.4%) presented with poor Eastern Cooperative Oncology Group Performance Status (ECOG-PS), 275 (60.3%) with elevated lactate dehydrogenase (LDH) level, 263 (57.7%) with extranodal involvement of 1 or more sites, and 64 (14.0%) with bulky mass. As a consequence, 211 patients (46.3%) were in high/high-intermediate International Prognostic Index (IPI) categories. 5 years overall survival (OS) was 66.2%, in total. EBV was detected in samples from 47 patients (10.3 %). The positivity was 10.6% (15 / 142) in patients of 60 years or younger, and 10.2 % (32 / 314) in those older than 60 years (p = 0.51). No differences in back ground date were found between EBV - positive and negative DLBCLs regarding age (median 66.5 vs. 64.8, P = 0.17), male sex (88.1% vs. 11.9%, P = 0.16), advanced stage (88.2% vs. 11.8%, P = 0.17), poor ECOG-PS (90.3% vs. 9.7%, P = 0.47), elevated LDH (89.5% vs. 10.6%, P = 0.48), extranodal sites of one or more (90.5% vs. 9.5%, P = 0.31), bulky mass (92.2% vs. 7.8%, P = 0.33), and higher IPI categories (88.6% vs. 11.4%, P = 0.29).
The prognosis was also not different between EBV-positive and negative DLBCLs. The 5 years OS was 42.6% for EBV-positive DLBCLs, and 56.4% for EBV-negative DLBCLs (P = 0.11). The same results were found for the younger (53.3% vs. 66.9%, P = 0.30) and the elderly patients (42.9% vs. 51.8%, P = 0.18).
Conclusion: In this practice based, uncontrolled study, EBV-positively wad not different in younger and elderly DLBCLs. Although EBV-positive DLBCL showed worse trend of prognosis, the difference was not statistically significant. The significance of EBV in DLBCL should be reconsidered in unbiased, large-scale patient date.
Suzuki:Chugai: Honoraria; Bristol-Myers Squibb: Honoraria; Kyowa Hakko kirin: Honoraria. Suzumiya:Chugai: Research Funding, Speakers Bureau; Astellas: Research Funding; Toyama Chemical: Research Funding; Eizai: Research Funding; Takeda: Speakers Bureau; Kyowa Hakko Kirin: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.