Abstract
Myeloproliferative neoplasms (MPN) are associated with an increased risk of arterial and venous thrombosis. Besides clinical factors (previous history of thrombosis, age > 60 years, cardiovascular risk factors), procoagulant phenotype, proadhesive properties of the endothelium and secretion of inflammatory cytokines, contribute to the pathogenesis of thrombosis in MPN. Pegylated interferon alpha (IFN) has obviously a great therapeutic efficacy on hematopoietic cell proliferation but its other biological effects particularly on hemostasis and inflammation have not been determined.
The aim of the study was to determine whether IFN impacts the biological profile including endothelial and platelet markers compared to MPN patients treated by hydroxyurea (HU) and non-treated (NT) patients.
Patients with polycythemia vera (PV) or essential thrombocythemia (ET) treated with IFN or HU or without any cytostatic drug were included. Platelet membrane glycoproteins and platelet activation were measured by flow cytometry. We evaluated shear-induced platelet aggregation (SIPA) at 4000 sec-1 that mimics stenotic arteries. We measured coagulation proteins by their activity and endothelial parameters (von Willebrand factor (VWF) antigen and activity, soluble thrombomodulin). Thrombin generation was measured in platelet poor plasma and platelet rich plasma. Platelet accumulation on immobilized collagen was measured using whole blood perfused at 1500 sec-1 in flow chambers. Statistical analysis was performed by ANOVA to compare the 3 groups of patients (p<0.05) and post-test Newman-Keuls to compare groups side-by-side (p<0.01).
Eighty-eight patients were included: 28 treated by IFN (20 PV and 8 ET), 38 treated by HU (27 PV and 11 ET) and 22 NT (6 PV and 16 ET). All patients were treated with aspirin 75 or 100 mg/day. Prior history of thrombosis occurred in 25.7% of ET and in 31.5% of PV. During the follow up (> 6months), only 1 arterial and 2 venous thrombosis were observed.
Hematological parameters and JAK2 V617F status was in the expected range in ET and PV patients.
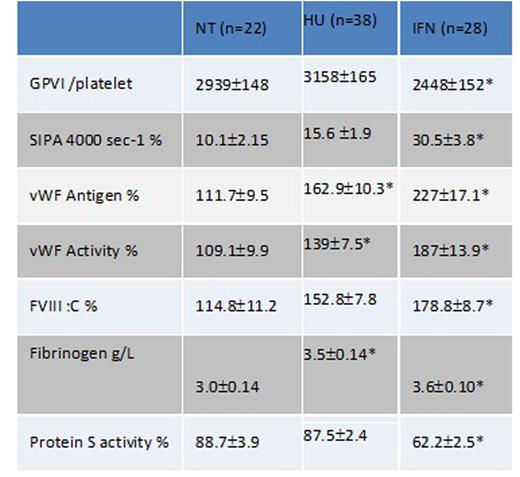
Surprisingly, we observed some significant effect of IFN on 1) platelets with a decreased GPVI expression compared to HU- and non-treated patients and increased levels of SIPA at 4000 sec-1. 2) endothelial cells with significantly increased levels of Willebrand antigen and activity. 3) coagulation parameters with decreased protein S activity and increased levels of factor VIII:C and fibrinogen (table 1). All the other parameters tested were similar in the 3 groups of patients.
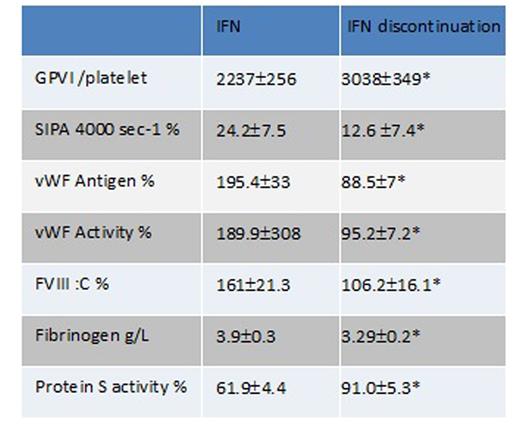
We had the opportunity to test 10 patients at least 6 months after IFN discontinuation. IFN was stopped for side effects in 6 patients, for complete molecular response in 2 and for normalization of hematological parameters in 2 others. GPVI expression, SIPA, VWF activity and antigen, protein S activity, FVIIIC and fibrinogen returned to levels similar to those of non-treated patients and were significantly different from the levels in IFN-treated patients (table 2). These results indicate that IFN was responsible for these biological modifications.
In conclusion, these unexpected data showing an increase of procoagulant and inflammatory markers in IFN-treated MPN patients could be considered as a part of IFN biological activity. Though minimal, these alterations could require more intensive preventive anticoagulation than aspirin in patients with heterozygous FV Leiden or FII G20210A mutation.
comparison of biological parameters in the 3 groups of patients. *p<0.01 compared to NT
comparison of biological parameters in the 3 groups of patients. *p<0.01 compared to NT
comparison of biological parameters before and after IFN discontinuation in 10 patients. *Wilcoxon test p<0.05
comparison of biological parameters before and after IFN discontinuation in 10 patients. *Wilcoxon test p<0.05
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.