Abstract
Background: Allogeneic Hematopoietic Stem Cell Transplantation (aHSCT) represents the only curative modality for unfavorable acute leukemia (AL) and myelodysplastic syndrome (MDS). Despite its curative intent, a significant number of recipients relapse. There is no standardized approach for the management of relapse following transplants and therapeutic options vary among centers, which represent a major challenge. Post transplant relapse is usually associated with a poor outcome while the impact of the treatment choice on health care resource utilization and survival is unknown. The objective of this study was to measure the health care resource utilization for the management of relapse following AHSCT and how the treatment choice impacted on survival.
Methods: A retrospective medical chart review was conducted at H™pital Maisonneuve-Rosemont (HMR) after research and ethic committee approval. Patients were selected using the Hematopoietic Stem Cell Transplant (HSCT) program database. Eligible patients were diagnosed with AL or MDS and relapsed following a HLA identical aHSCT between January 1st 2011 and December 31st 2014. Patients' and disease characteristics as well as relapse-related health care resource utilization were collected from the date of transplant relapse diagnosis until death or last follow-up.
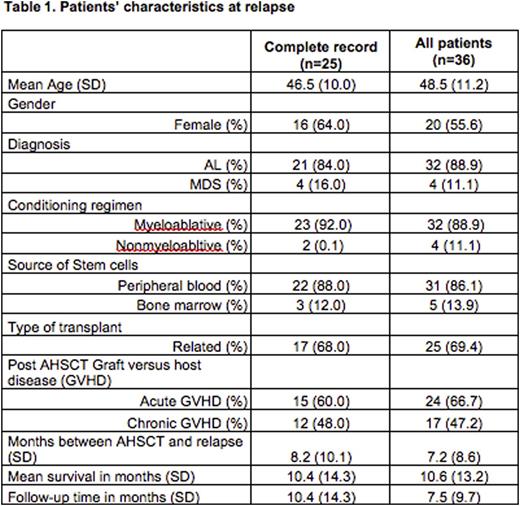
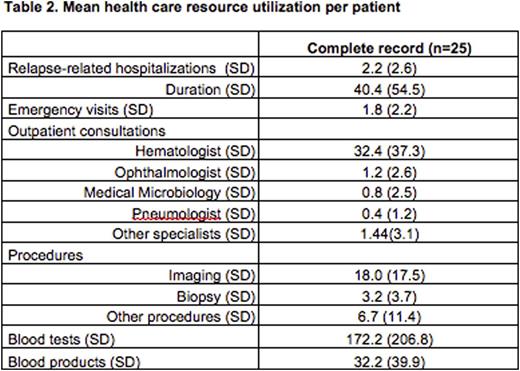
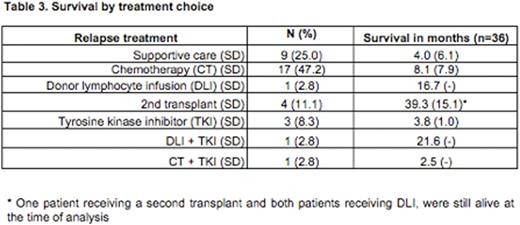
Results: During the study period, of the 645 HSCT performed at HMR, 303 were allogeneic. A total of 36 patients who relapsed met the inclusion criteria and were included in the survival analysis. Healthcare resource utilization analysis was conducted on the 25 patients for whom complete records were available. Patients' characteristics at relapse, mean health care resource utilization per patient and survival by treatment choice are presented in tables 1, 2 and 3 respectively. The mean time from relapse to death was 10.6 months (SD=13.2). Relapse-related hospitalization duration represented on average 20.3% of patients' follow-up period (SD=26.0). For a mean follow-up time of 9.5 months (ranged from 6 days to 4.8 years), the mean number of relapse-related hospitalization was 2.2 per patient (SD=2.6). The mean length of stay was 40.4 days per patient (SD=54.5). The mean hematologist consultation number was 32.4 per patient (SD=37.3
Conclusion: Relapse following AHSCT is associated with a poor prognosis and survival and significant use of health care resources. Aggressive treatment rarely leads to a second transplant. Innovative approaches should be developed to address this unmet medical need. Healthcare resources devoted to the care of patients in relapse post AHSCT provide a comparative basis for the development of cellular therapy.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.