Abstract
Background: The use of tyrosine kinase inhibitors (TKIs) in the treatment of Philadelphia chromosome (Ph+) or BCR-ABL positive acute lymphoblastic leukemia (ALL) has improved remission rates allowing more eligible patients to proceed on to allogeneic hematopoietic stem cell transplantation (alloHSCT). Since many patients relapse following alloHSCT, some guidelines have recommended TKIs post alloHSCT (Couban, 2014, Giebel, 2016). Although some studies have demonstrated the benefits of this strategy, others have indicated that, owing to the immunomodulatory effects of TKIs, this approach may be harmful, leading to higher relapse rates. Given this uncertainty, we conducted a systematic review and meta-analysis of published studies comparing the outcomes of patients post alloHSCT who did or did not receive TKIs.
Methods: We searched MEDLINE, EMBASE, Cochrane Database of Systematic Reviews, Cochrane Central Register of Controlled Trials, ACP Journal Club, Scopus and conference abstracts focusing on the period during which TKIs were available (2000 to March 2016). Studies were included if they were retrospective or prospective cohort/randomized studies of adult patients with Ph+ or BCR-ABL+ ALL who underwent alloHSCT and received post-transplant TKIs. Studies that did not include a comparative group of patients who did not receive TKIs, duplicate studies, abstracts later published and studies of only pediatric patients were excluded from further analyses. Two reviewers with ALL expertise independently evaluated all abstracts and performed study selection.
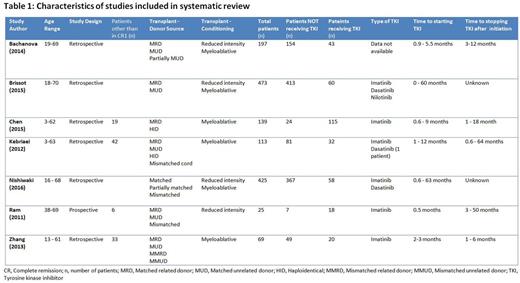
Results: The literature search identified 868 unique references, 195 of which were reviewed in detail. Seven studies, 6 retrospective and 1 prospective, comprising 1441 patients met all inclusion criteria (Table 1). Three studies contained one or more pediatric patients and four included patients beyond first complete remission including some with hematological relapse at the time of alloHSCT. All studies had a mix of donor sources including matched related, matched unrelated, mismatched related and mismatch unrelated. Pre-transplant conditioning was myeloablative in 3, reduced intensity in 1 and a combination of the two in the remaining 3 studies.
TKIs were administered prophylactically (prior to hematological or minimal residual disease relapse) or pre-emptively (prior to hematological relapse). Data on the TKI used was not available in one study. Amongst the remaining 6 studies, imatinib at 400 - 600mg was the most commonly used TKI with dasatinib being used in 3 studies and nilotinib in 1 study. TKIs were initiated 0.5 - 60 months after alloHSCT and continued for 1-64 months after initiation.
Overall, 346 patients received a TKI post alloHSCT while 1095 patients did not. Using a fixed effects model there was no difference in the relapse free survival (HR =0.838, 95% CI 0.678 - 1.036, p=0.102) or overall survival (HR=0.868, 95% CI 0.675 - 1.117, p=0.27) for those who received a TKI compared to those who did not. In contrast, there was a significant increase in relapse rates for those who were treated with TKI post-HSCT (HR 1.204, 95% CI 1.044 - 1.387, p=0.011).
Conclusions: While there are compelling theoretical reasons to recommend TKIs post alloHSCT (Couban, 2014), this meta-analysis suggests that their use is not associated with improvements in overall survival or relapse free survival and may be associated with higher relapse rates. However, given the heterogeneous nature of the studies, these results must be viewed with caution. Nonetheless, the results are compelling and highlight the need for larger prospective controlled studies evaluating the role of TKI post alloHSCT in patients with Ph+ ALL.
Liew:Novartis: Honoraria, Membership on an entity's Board of Directors or advisory committees; BMS: Membership on an entity's Board of Directors or advisory committees.
Author notes
Asterisk with author names denotes non-ASH members.