Abstract
Introduction: Despite decades of research, acute myeloid leukemia (AML) remains difficult to treat, and clinical trials are recommended as first line therapy by the NCCN. Although many new drugs show promise in early trials, further experience often does not confirm these results. One possible explanation is that patients on trials are not broadly representative. Here, we retrospectively compared characteristics, response, and survival in patients given the same investigational regimens according to whether treatment was given on versus off study.
Methods: Patients treated for AML or high-risk MDS at FHCRC/UW between 2008 and 2015 were included. Investigator-initiated protocols for newly diagnosed (ND) and relapsed / refractory (RR) disease were included if ≥15 patients were treated off study. Analyses used Fisher's exact test, Wilcoxon rank sum test, the Kaplan-Meier method, and Cox multivariate models.
Results: 165 ND patients received either escalating doses of G-CLAM or idarubicin, cytarabine, and pravastatin while 243 RR patients received G-CLAM, decitabine-primed MEC or G-CLAC. Overall, 216 were treated on study and 192 were treated off study; reasons for the latter were: protocol not open (n=64), high treatment-related mortality score (n=21), poor health / organ function (n=26), physician or patient preference (n=25), lack of insurance (n=6), and not identified (n=50). No significant differences were found in age, gender, cytogenetic risk, or primary vs. secondary leukemia, but those treated on study in dose escalation protocols were more likely to receive higher doses. RR patients treated off study had typically received more salvage regimens.
The 86 ND patients treated on study had higher rates of CR/CRi (90% vs. 64%, P<0.001) and CR without MRD (67% vs. 36%, P<0.001) than the 79 treated off study. These associations remained after adjusting for treatment date, age, gender, secondary leukemia, adverse cytogenetics, and regimen type (OR 3.99 [95% CI: 1.60-9.97] and OR 2.93 [1.39-6.17] respectively). In contrast, neither CR/CRi nor CR without MRD rates differed for RR patients treated on (n=130) or off (n=113) protocol: 52% vs. 41%, P=0.07 and 28% vs. 19%, P=0.14. The same applied after adjusting for the above factors as well as duration of first remission and salvage number: OR 1.79 [0.95-3.40] and OR 1.73 [0.80-3.71].
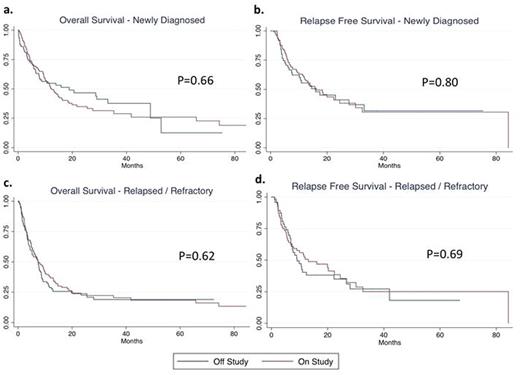
Despite having higher remission rates, ND patients treated on vs. off study had comparable OS, and, among patients achieving remission, RFS (Figure 1a and 1b). After multivariate adjustment, there remained no association with OS (HR 0.87 [0.52-1.47]) or RFS (HR 0.96 [0.53-1.75]). Survival outcomes were also similar regardless of study assignment among RR patients (Figure 1c and 1d), in both univariate and multivariate analysis (OS, HR 0.82 [0.58-1.17]; RFS HR 0.72 [0.39-1.34]). Patients treated on or off dose escalation protocols at the maximum tolerated dose were no more likely to achieve remission or have longer survival, and incorporating subsequent allogeneic transplant as a time-varying covariate did not significantly affect outcomes.
Conclusions: The higher response rates in ND patients treated on vs. off study suggests a measure of selection bias unrelated to readily assessable covariates, while the fundamental determinant of response in RR patients and survival in all patients appears to be unfavorable disease features (adverse cytogenetics, number of prior salvages, duration of CR1). Routine reporting of off study data for investigator-initiated studies could provide a clearer picture of regimen response rates and would grant further insight into the effects of selection bias.
Kaplan-Meier curves for on and off study patients depicting OS and, among patients achieving remission, RFS. Outcomes are depicted in ND patients (a and b) and in RR patients (c and d).
Kaplan-Meier curves for on and off study patients depicting OS and, among patients achieving remission, RFS. Outcomes are depicted in ND patients (a and b) and in RR patients (c and d).
Othus:Glycomimetics: Consultancy; Celgene: Consultancy. Shadman:Gilead: Honoraria, Research Funding; Pharmacyclics: Honoraria, Research Funding; Emergent: Research Funding; Acerta: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.