Abstract

Background Routine diagnostic lumbar puncture is not recommended in adult patients with acute myeloid leukemia (AML) without Central Nervous System (CNS) symptoms and little is known about the incidence of CNS involvement and its impact on survival in these patients. Furthermore, several studies have demonstrated that flow cytometry (FCM) is superior to conventional cytology (CC) for detection of CNS involvement in lymphoproliferative disorders but the role of this approach for the investigation of cerebrospinal fluid (CSF) in AML is unknown.
Design and Methods The aims of our study were 1) to determine the incidence of occult/manifest CNS disease in a homogenous series of AML patients; 2) to correlate CNS disease with clinico-biologic parameters; 3) to examine the impact of CNS involvement on outcome. CSF samples were collected from 98 newly diagnosed AML patients, 62 males and 36 females, median age 53 years (range 18-75). Sixty-five and 33 patients aged <60 and>60 years, respectively.Seventy-one patients received standard and 22 high-dose-ARA-C-based regimens, 5 supportive care. All of 98 CSF samples were examined by CC whereas 90 (91%) also by FCM. CC positivity was defined as unequivocal morphologic evidence of leukemic blast in CSF and/or white blood cells count (WBCc) ≥ 5/µl with less than 10 erythrocytes/µl. A cluster of at least 10 phenotypically abnormal events was regarded as a proof of FCM positivity.
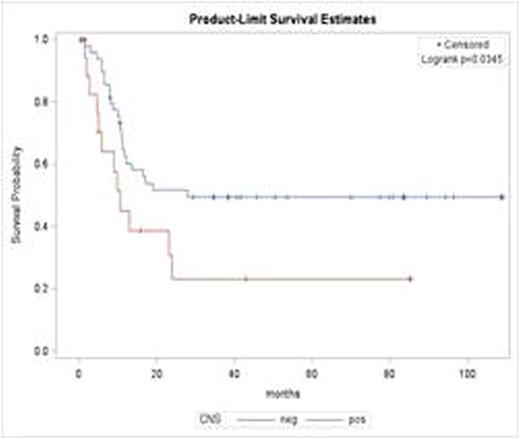
Results Sixty-seven patients were CNS negative (CNS-) while thirty-one (31%) were CNS positive (CNS+). Among the last, 10 (10%) were positive on both CC and FCM (manifest CNS+) and 21 (21%) only on FCM (occult CNS+). There was an equal male/female distribution among CNS- and CNS+ patients, as well as median age (52 years, range, 20-71, vs 56 years, range, 18-75, p=NS) and WBCc(27.5 x109/L, range, 1,20-223 x109/L, vs. 11,6 x109/L, range, 0,70-315 x109/L, p= NS) were similar in both groups. Instead, higher levels of lactate dehydrogenase (LDH) were observed among CNS+ than CNS- patients (p=. 01). Forty-seven patients (48%) had monoblastic/monocytic or myelomonocytic AML and belonging to one of these categories was significantly associated with a condition of CNS positivity (55% vs 45%, P = 002). Cytogenetic/genetic data were available in 82/98 (84%). Twenty-for patients (29%), 33 (39%), 12 (14%) and 12 (14%), belonged to the category of favorable, intermediate-I, intermediate-II, and adverse karyotype, respectively. Cytogenetic/genetic characteristics did not differed significantly between CNS+ and CNS- patients. Overall, response rate was 70%, with complete remission rate being not statistically different between CNS+ and CNS- patients (69% vs 81% p= NS). Five-year DFS and OS were found to be significantly shorter in occult or manifest CNS+ patients than in those CNS- (23% vs 50% p= .03 and 19% vs 46%, p=.02, respectively)(Figure 1A and 1B). The prognostic variables achieving a statistical significance in univariate analysis (CNS status, age , WBCc, favorable vs adverse karyotype) were challenged in a multivariate model to determine to what extent they affected treatment outcome. In multivariate analysis, CNS positivity was found to be independently and significantly associated with a shorter duration of DFS.(p=.03 HR= 0.46). Age >50 years was found to be the only independent prognostic factor affecting OS (p=.01 HR= 2.26).
Conclusion Our data suggest that incidence of CNS involvement in newly diagnosed AML pts is higher than expected. Regardless of neurologic symptoms, manifest and occult CNS positivity should always be sought at diagnosis since it may affect outcome and influence therapeutic decision. Further prospective studies on larger series are warranted to confirm this data.
Lo Coco:Teva: Consultancy, Honoraria, Speakers Bureau; Lundbeck: Honoraria, Speakers Bureau; Novartis: Consultancy; Baxalta: Consultancy; Pfizer: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract