Abstract
Background: Therapy for children with acute myeloid leukemia (AML) is intensive and treatment-related mortality (TRM) occurs in about 5 to 10% of patients. Previous data illustrated that obese children and adolescents with AML treated according to CCG 2961 were more likely to experience TRM, with HR 2.66 (95% CI 1.38-5.11; P = 0.003), when compared to middleweight patients. Since this trial, the backbone of AML chemotherapy and supportive care have changed and thus, it is unknown whether the impact of obesity persists in contemporary trials. The objective was to determine whether obesity was associated with increased TRM, reduced survival and prolonged compared to middleweight patients with AML.
Methods: AAML0531 enrolled patients between August 14, 2006 and June 15, 2010. For this analysis, we included patients 0 to 18 years of age with de novo AML. Chemotherapy consisted of 5 cycles of chemotherapy and patients were randomized to receive or not receive gemtuzumab once during Induction I and Intensification II. Best allogeneic donor hematopoietic stem cell transplantation (HSCT) was recommended for those with > 15% bone marrow blasts after Induction I in those without favorable risk cytogenetics and poor risk cytogenetics irrespective of response following Induction I. Matched family donor HSCT was recommended for those with good response after Induction I with standard risk cytogenetics and an available donor.
Obesity was defined using definitions from the Centers for Disease Control and Prevention (CDC). Underweight was defined as a body mass index percentile less than 5th percentile, and obese 95th percentile and greater. Categories were determined using z-scores for the weight-for-height data for those 0 to 2 years of age.
All outcomes were censored at the time of HSCT. The primary outcome was TRM, defined as death as first event occurring on therapy or within 30 days of going off therapy. Cumulative incidence of TRM was estimated treating relapse and failure as competing events. Kaplan Meier analysis was conducted for overall survival (OS), event free survival (EFS), and disease free survival (DFS). Cumulative incidence of relapse rate (RR) was estimating treating deaths as competing events.
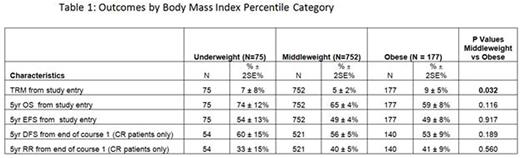
Results: There were 1004 patients included. When comparing middleweight and obese patients, there was no significant difference in gender (P=0.814), white vs non-white race (P=0.116), cytogenetic risk group (all P>0.05) or MRD positivity after Induction 1 (P=0.750). The median age was higher for obese patients (12.0 vs 9.4 years; P=0.007 years) compared with middle weight patients. The proportion of patients who were Hispanic or Latino patients was higher among obese compared with middle weight patients (28% vs 17%; P=.001). Survival outcomes are shown in Table 1.
When evaluating median time to neutrophil recovery, obese patients, when compared to middleweight patients, had shorter duration of neutropenia for cycles 1-3 (P<0.05).
Conclusions: TRM rates continue to be higher for obese patients treated with contemporary AML protocols. Toxicity is not mediated through prolonged neutropenia. Future work should compare the rate of toxicity among obese versus non-obese patients and evaluate the impact of underweight status.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal