Abstract
Introduction: Conventional allogeneic hematopoietic cell transplantation (allo-HSCT) is an established therapy for the treatment of patients (pts) with acute myeloid leukemia (AML) and myelodysplastic syndrome (MDS). CD34 selected allo-HSCT has been shown to yield similar survival rates as unmodified transplant but with significantly lower risk for acute and chronic GVHD. This type of transplant is done mostly in the context of a myeloablative conditioning (MAC) regimen and a common chemotherapy regimen is busulfan (bu), melphalan and fludarabine. The aim of this study is to evaluate PK directed bu dosing strategy in pts with MDS and AML undergoing CD34 allo-HSCT.
Patients and Methods: This was a retrospective analysis performed at Memorial Sloan Kettering Cancer Center and included 166 adult pts with advanced MDS (RAEB-1 and higher) or AML who underwent CD34 selected allo-HSCT between 2000-2014. Pts who were conditioned with bu at a total daily dose of 3.2mg/kg (given q6 or q24 over 3 days), melphalan 140mg/m2, fludarabine 125mg/m2 and ATG were included. Median age was 63 yrs (28-73). There were 76 women (46%). HCT-CI was ≥3 in 70 pts (43%). There were 66 pts with MDS (40%). Donors were HLA matched in 129 pts (37% related and 63% unrelated) or mismatched in 37 pts, all unrelated. Pharmacokinetics were assessed after the first bu dose and adjustment was made to achieve a targeted total daily busulfan AUC of 4100-5200 min*umol/L (goal 4700 min*umol/L). CD34 selection of granulocyte colony-stimulated factor (G-CSF) -mobilized PBSCs was accomplished by positive selection of CD34+ stem cells using the ISOLEX 300i Magnetic Cell Separator (Baxter, Deerfield, IL) and then sheep RBC rosette depletion for 58 pts (35%) and since October 2010 the CliniMACS CD34 Reagent System was used for 109 pts (65%) (Miltenyi Biotech, Gladbach, Germany). Association between categorical variables was tested using Fisher's exact test, HSCT outcomes and survival outcomes were examined using log-rank test, Grey's test and competing risk regression by Fine and Grey's method.
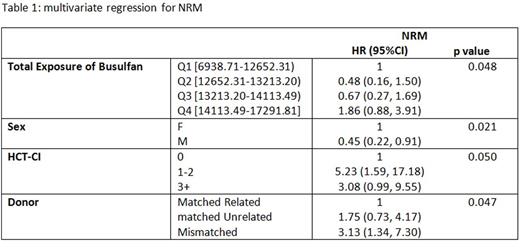
Results: The median initial bu dose was 60mg for q6h dosing (19-82) and 240mg for q24h dosing (170-310). In 96 pts (58 %) there was a need for dose adjustment after the first PK resulted; dose increase was required in 59 pts (36%). The median total bu exposure for all pts was 13213 min*umol/L (6938-17291). After first dose PK adjustments, range of total exposure with 1st quartile (Q1) was 6938-12365, 2nd quartile (Q2) 12652-13213, 3rd quartile (Q3) 13213-14113 and 4th quartile (Q4) 14113-17291. Pt characteristics (age, gender, HCT-CI), disease characteristics, type of pre-transplant treatment, as well as donor status were not associated with first bu AUC. None of these factors were associated with total bu exposure other than gender: females were more likely to have lower bu exposure (Q1), while males were more likely to have higher exposure (Q2 and Q3) and male and female distribution was similar in Q4 (p=0.025). Univariate analysis of clinical outcomes by bu exposure quartiles showed worse NRM for pts in Q4 (14113.49-17291.81): day 100 cumulative incidence of NRM was 11.9% (95% CI: 2-21.8), and by 1 year 33.5% (95% CI: 19%-48.1%), p=0.036. It remained significant in multivariable regression analysis after adjusting for other parameters that were found to predict for NRM including donor status, gender and HCT-CI HR of 1.86 (95% CI: 0.88-3.91), p=0.048 (Table 1).
Conclusions : In this cohort of MDS and AML patients undergoing CD34 allo-HSCT results suggest that total bu exposure higher than 14113 min*umol/L (Q4) was associated with increased NRM. Lower bu exposure was not associated with increased relapse or decreased survival. We were not able to identify any patients or disease characteristics that were associated with bu doses. Targeting a lower total exposure of bu between 12652-14113 umol*min/L or total daily bu AUC of 4200-4700 umol*min/L could result in a decreased risk of NRM in this patient population.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.