Abstract
Introduction: Reduced-intensity conditioning (RIC) regimens have been increasingly used in allogeneic hematopoietic stem cell transplantation (allo-HCT), because they can reduce non-relapse mortality in comparison with standard myeloablative conditioning regimens and allow previously ineligible patients such as older patients and patients with comorbidities to receive allo-HCT. However, the optimal RIC regimen in allo-HCT remains unclear. Therefore, we conducted a nationwide retrospective study to compare the transplant outcomes between fludarabine/busulfan (FB) and fludarabine/melphalan (FM) regimens which are two most widely used RIC regimens for allo-HCT.
Methods: We retrospectively analyzed 2008 patients aged 50 years or older with acute myeloid leukemia (AML) (n=1219), acute lymphoblastic leukemia (ALL) (n=209), or myelodysplastic syndrome (MDS) (n=580) who underwent allo-HCT using fludarabine/busulfan (FB) or fludarabine/melphalan (FM) between 2001 and 2014. The patients who underwent cord blood transplantation were excluded in this study, but those who received low dose of total body irradiation in addition to the FB or FM regimen were included. Acute leukemia in the first or second remission and MDS excluding refractory anemia with excess blasts or leukemic transformation were defined as standard-risk diseases. Clinical data for these patients were obtained from the Transplant Registry Unified Management Program (TRUMP), which includes clinical data of HCT performed in Japan. We compared the outcomes between FB2 (busulfan at 8 mg/kg po or 6.4 mg/kg iv, n=738), FB4 (busulfan at 16 mg/kg po or 12.8 mg/kg iv, n=749), and FM140 (melphalan at 140 mg/m2, n=521).
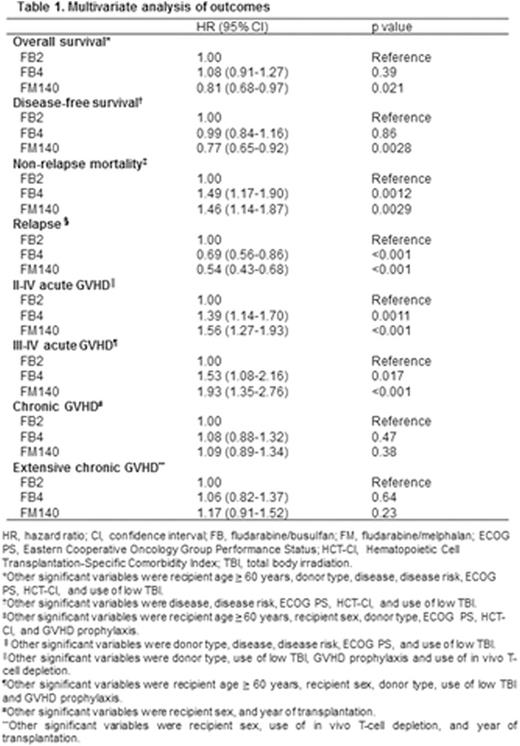
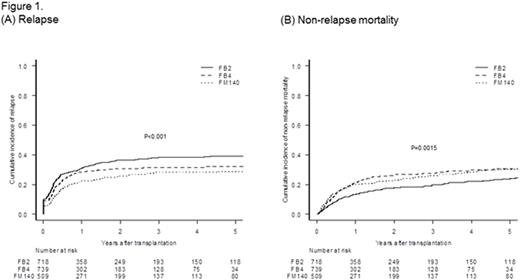
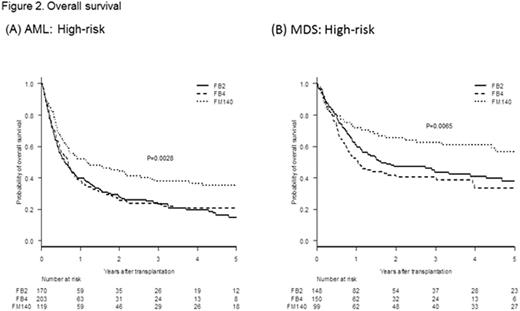
Results: The median ages were 60 (50-74), 60 (50-75), 59 (50-71) years in the FB2, FB4, and FM140 groups, respectively. The cumulative incidences of grade II-IV and III-IV acute GVHD were 30.7% (95% confidence interval (CI), 27.3-34.1%) and 10.1% (95% CI, 8.0-12.4%), 36.8% (95% CI, 33.3-40.2%) and 12.5% (95% CI 10.2-15.0%), and 39.3% (95% CI, 35.0-43.5%) and 15.2% (95% CI, 12.2-18.4%) in the FB2 group, the FB4 group, and FM140 group, respectively (p=0.0061 and p=0.050). The incidence of relapse at 3 years was higher in the FB2 group (38.2%; 95% confidence interval (CI), 34.5- 41.9%) than the FB4 group (31.5%; 95% CI, 28.0- 35.0%) or the FM140 groups (28.3%; 95% CI, 24.2- 32.4%, p<0.001, Figure 1A). Conversely, the incidence of non-relapse mortality was lower in the FB2 group (19.7%; 95% CI, 16.7- 22.9%) than the FB4 group (27.4%; 95% CI, 23.9- 30.9%) or the FM140 group (26.2%; 95% CI, 22.3- 30.3%, p=0.0015, Figure 1B). Overall survival (OS) at 5 years in patients with high-risk AML and MDS in the FM140 group (35.3%; 95% CI, 26.2-44.6% and 57.0%; 95% CI 45.2-67.2%) was superior to that in the FB2 group (15.2%; 95% CI 9.3-22.3% and 38.1%; 95% CI 28.8-47.2%) or FB4 group (20.8%; 95% CI, 14.5- 27.8% and 33.8%; 95% CI 23.9-43.9%) (p=0.0028 and p=0.0065, Figure 2A, B), although OS in patients with standard-risk AML or MDS did not differ among the 3 groups. On the other hand, no statistically significant differences were found in OS in patients with standard- and high-risk ALL in the FB2, FB4, and FM140 groups (OS at 5 years in standard-risk ALL patients: 54.9%; 95% CI 40.2-67.4%, 33.6%; 95% CI 10.9-58.4%, and 49.2%; 95% CI 34.8-62.1%; p=0.32, and OS at 3 years in high-risk ALL patients: 20.8%; 95% CI 0.9-59.5%, 0%; 95% CI NA-NA, and 11.3%; 95% CI 0.7-38.3%; p=0.54, respectively). In multivariate analysis (Table 1), the non-relapse mortality rate was significantly higher in the FB4 and FM140 groups than that in the FB2 group (hazard ratio (HR) 1.49; 95% CI 1.17-1.90; p=0.0012 and HR 1.46; 95% CI, 1.14-1.87; p=0.0029). On the other hand, the relapse rate was significantly lower in the FB4 and FM140 groups than that in the FB2 group (HR 0.69; 95% CI, 0.56-0.86; p<0.001 and HR 0.54; 95% CI, 0.43-0.68; p<0.001), and overall survival (OS) was better in the FM140 group than in the FB2 group (HR 0.81; 95% CI, 0.68-0.97; p=0.021), although there were no significant differences between the FB4 and FB2 groups (HR 1.08; 95% CI, 0.91-1.27; p=0.39).
Conclusion: FM140 was associated with better OS in patients with high-risk AML and MDS than FB2 because of lower relapse rate and FB4 was not superior to FB2 in OS, although OS in patients with standard-risk disease did not differ among the 3 groups. A large prospective study is warranted to confirm these findings.
Kako:Otsuka Pharmaceutical: Honoraria. Kanda:Otsuka Pharmaceutical: Honoraria, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.