Abstract
Background: Over 10,000 new cases of myelodysplastic syndrome (MDS) are diagnosed in the US annually (MA X, Cancer 2007). Hypomethylating agents (azacitidine and decitabine), immunomodulating drugs (lenalidomide) and erythropoietin stimulating agents (epoetin α and darbepoetin) have been approved for more than a decade for the treatment of MDS. However, changes in overall outcome after the approval of these treatments are unknown. We used the National Cancer Data Base (NCDB), a nationwide oncology registry covering 70% of the US cancer population to answer these questions.
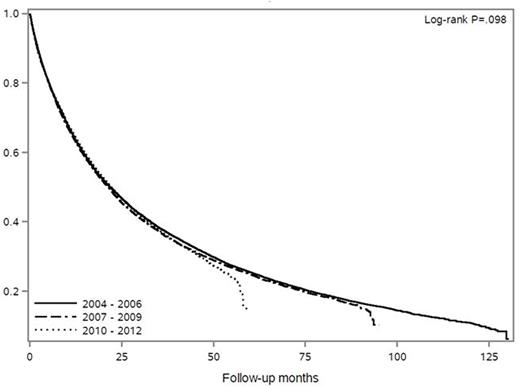
Methods: We identified patients with MDS diagnosed from 2004-2013 using ICD-O-3 codes 9980-9983 and 9985-99912. Overall survival (OS) was estimated using the Kaplan-Meier method. We compared OS using the log-rank test according to demographic subgroups (sex, age [<40, 41-65, and ≥65 years], race [White, Black, Native American, Asian/Pacific Islander, and other], and ethnicity) across years of diagnosis (Period 1: 2004-2006, Period 2: 2007-2009, and Period 3: 2010-2013).
Results:
i) Characteristics: There were 54,953 MDS patients in our study. The median age at diagnosis was 76 years (78.7% older than 65) and 44% were females. White race (88.9%) was the most common, followed by black (7%). Four percent were Hispanics. A third (30.8%) of all patients were treated in academic centers. Three quarters (75.8%) had either Medicaid or Medicare insurance.
ii) MDS Subtypes: 5q Syndrome was seen in 2008 cases (3.7%) while the most common subtype was MDS-Unclassifiable (U) (55.6%). Therapy related MDS (t-MDS) was seen in 1125 cases (2%), however coding for t-MDS was discontinued in 2009. Refractory anemia (RA), refractory anemia with ring sideroblasts (RARS), refractory cytopenia with multilineage dysplasia (RCMD), and refractory anemia with excess blasts were seen in 9%, 7.6%, 6%, and15.6%, respectively.
iii) OS: Compared to their counterparts, patients who were male, older, had a diagnosis of RAEB, covered by Medicare insurance, and treated at non-academic centers had the worse OS (all P <0.001). Across Periods 1-3, we did not see improvement in OS among demographic subgroups except for those who were <40 years old (P=0.03).
Conclusions: In the past decade, the overall outcome of MDS did not improve despite the advent of new therapies. More than half of the cases were classified as MDS-U reflecting the difficulty of subtyping MDS based on World Health Organization classification. We found disparity in outcomes by demographics and type of treatment facility. This is the largest study of MDS outcome to-date and should help in understanding the gaps and areas that need future research.
Al-Kali:Onconova Therapeutics, Inc.: Research Funding; Celgene: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.