Abstract
MM is a heterogeneous disease. The International Staging System (ISS) and the revised-ISS (R-ISS) can be used to stratify patients in terms of risk of mortality in newly-diagnosed MM (NDMM) however; there is less understanding of the predictors of OS in the relapsed setting. This retrospective analysis of the Registry of Monoclonal Gammopathies database, which covers ~80% of all Czech patients with MM, was designed to explore how predictors of OS differ between initiation of first- and second-line treatments, in order to further understand patient heterogeneity as the disease progresses.
Eligible patients initiated first-line treatment for symptomatic MM between May 2007 and April 2016. Factors considered prognostic of OS in both NDMM and relapsed/refractory MM were identified from targeted literature searches. Predictors of OS in second-line treatment included historical parameters that reflect outcomes to previous therapy. OS data was then fitted with multiple Cox-regression models. Backward selection was performed using Akaike's Information Criterion (AIC) as selection criterion.
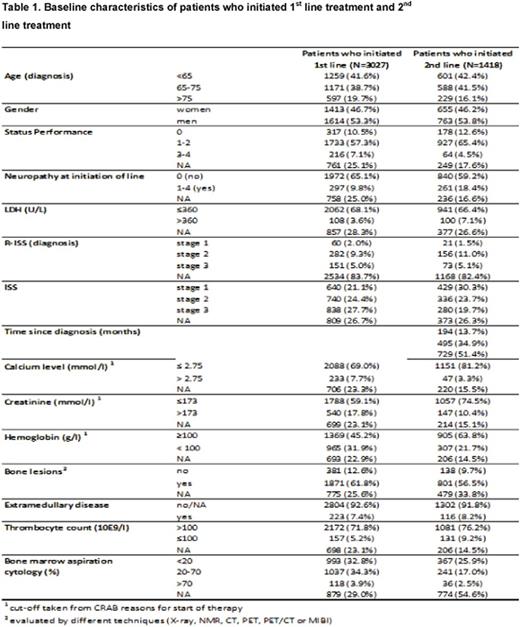
Patient characteristics at both first- (N=3027) and second-line (N=1418) treatment initiation are presented in Table 1. Comparison of these characteristics shows that as patients progress, on average their profile becomes less severe (e.g. ISS stage III 28% vs 20% in first- and second-lines, respectively), mainly explained by the dropout rate between first- and second-line treatment (Raab et al 2016) as patients either died or did not continue therapy due to adverse prognosis.
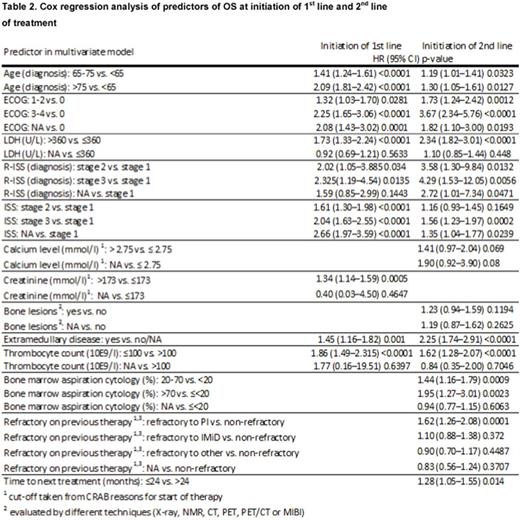
Median OS (95% CI) from initiation of first- and second-line treatment was 49.9 (46-54) and 27.6 (25-30) months. Results of OS predictive variables are shown in Table 2. Predictors of OS differ between initiation of first-line versus second-line therapy, both in terms of type of predictor as well as strength. At initiation of first-line, calcium level, bone lesions and bone marrow aspiration cytology were not significant predictors of OS, however they became significant at initiation of second-line or were selected by backward selection procedure. At initiation of second-line, historical parameters defining outcomes of prior treatments remained strong predictors, however only refractory status to prior bortezomib [HR=1.626 (1.267-2.087 p=0.0001)] and time to next treatment (TTnT) [HR=1.280 (1.051-1.559, p=0.014)] were significant predictors of OS. The significance of prediction of age and Eastern Cooperative Oncology Group (ECOG) performance status remained in both settings, with a lower impact of age in second-line treatment. Data for cytogenetics was not collected for initiation of second-line, however it is included in the R-ISS component. Although only measured at diagnosis, it remained a significant predictor in both settings (N.B. this variable had 82% missing values). Restaging of ISS at initiation of second-line was predictive, especially for those ISS III vs ISS I, HR=1.56 (1.23-1.97 p=0.0002). Additionally, lactate dehydrogenase (LDH), which is also a component of R-ISS was significant in both settings with as stronger effect in second-line. Elements normally considered predictive of OS at initiation of second-line did not appear in the final model: prior stem-cell transplant status or time-to-progression of previous therapy, perhaps explained by age and TTnT, respectively. Creatinine level was not significant at initiation of second-line, perhaps as patients with renal impairment during first-line treatment may not receive second-line treatment.
This real-world analysis of data from Czech patients revealed that predictors of OS differ between initiation of first- and second-line treatments. Prediction of OS in the relapsed setting should consider patient-related factors (age, ECOG), factors reflecting the disease activity and severity (LDH, bone lesion, calcium level) as well as historical elements, including those that were dependent on patient experience in the first treatment line (treatment response and duration of response). Additionally, there seems to be value in reclassification of patients in terms of severity at the relapse setting in order to improve prognosis and treatment selection in the relapsed setting.
Hájek:Takeda: Consultancy; Amgen: Consultancy, Honoraria, Research Funding; Celgene: Consultancy, Research Funding; BMS: Honoraria; Janssen: Honoraria. Jiri:Amgen: Consultancy. Walter:Amgen: Consultancy. Maarten:Amgen: Consultancy. Lucy:Amgen: Employment, Other: Amgen Stock. Marco:Amgen: Employment, Other: Holds Amgen Stock. Lucie:Amgen: Consultancy. Sebastian:Amgen: Employment, Other: Holds Amgen Stock.
Author notes
Asterisk with author names denotes non-ASH members.