Abstract
The assessment of pre-transplant comorbidities is crucial for risk-stratification and is a tool to guide clinical decisions in hematological malignancy patients (pts) undergoing evaluation for stem cell transplantation (SCT). The HCT-CI scale is commonly used to identify high risk patients pre-transplant as it is highly predictive of non-relapse mortality (NRM), severity of graft versus host disease and survival after allogeneic SCT (Sorror et al, Blood 2005; Sorror et al, Blood 2014). However, its role in ASCT remains undefined. In a Center for International Blood and Marrow Transplant Research analysis, HCT-CI score of ≥3 was prognostic for higher NRM and overall mortality in ASCT patients (Sorror et al, Biol. Blood Marrow Transplant 2015), but other single institution studies have failed to confirm this observation in lymphoma patients (Jaglowski et al, Bone Marrow Transplant 2014; Dahi et al, Biol. Blood Marrow Transplant 2014; Hosing et al, Ann. Oncol. 2008). No study has correlated HCT-CI with psychosocial functioning in the setting of ASCT.
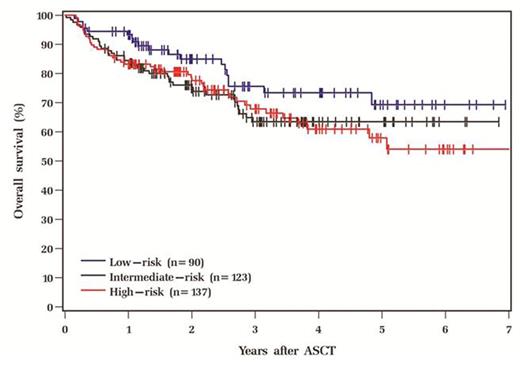
We conducted a retrospective study of 350 patients with Hodgkin (N=70) and non-Hodgkin Lymphoma (N=280) who underwent ASCT at our institution from January 2009 to June 2015. Based on their HCT-CI score, patients were categorized into low risk (score 0, N=90), intermediate risk (score 1-2, N=123) and high risk (score ≥3, N=137). Psychosocial Assessment of Candidates for Transplantation (PACT) scale (0-4: 0 being poor candidate for procedure and 4 being excellent candidate) (Foster et al. BMT 2009) was used for pre-transplant psychosocial risk assessment and was available for 235 pts. We analyzed the impact of HCT-CI on transplant outcomes and its correlation with PACT scores.
Our cohort was predominantly male (63%), and Caucasian (93%) with a median age of 55 years (range 20-78). The majority of the pts (96%) had good performance status with an ECOG of 0-1. The primary diagnosis was NHL in 80%, with mostly advanced stage disease (80%), and no B symptoms (93%). Median time from diagnosis to ASCT was 16 months with 75% of the pts having received ≤2 prior therapies. The median annual income based on zip code was $49406 (range $18753-127312). Disease status prior to transplant was CR/PR in 93% of the subjects. Patient and disease characteristics were comparable among the 3 HCT-CI risk groups. Higher HCT-CI risk category was associated with a lower median household income (p=0.012), higher LDH (p=0.004), more days of apheresis (p=0.026) and lower CD34+ dose x106/kg (0.046). In relation to PACT scores, higher HCT-CI was associated with poor mental health (p<0.001), decreased coping skills (p<0.001), unhealthy lifestyle habits/sedentary life (p<0.001), decreased compliance with medications/medical advice (p=0.014) and inadequate medical/transplant knowledge (p=0.017) and lower final PACT score (p<0.001). Median follow up was 35 months with 100 observed deaths, of which 72 were attributed to relapse. The 5 year estimated relapse rate, NRM, relapse free survival (RFS) and overall survival (OS) in our cohort were 42%, 11%, 49% and 62% respectively. On univariate analysis, there was no significant difference between high vs. low/intermediate HCT-CI scores on 30 day readmission rates (OR 1.24, p=0.61), 100 day mortality (OR 1.12, p=0.86), incidence of secondary malignancy (HR 0.41, p=0.17), relapse rate (HR 0.92, p=0.64), relapse mortality (HR 1.35, p=0.20), NRM (HR 0.86, p=0.71), OS (HR 1.2, p=0.37) or RFS (HR 0.98, p=0.92). Though not statistically significant, the intermediate risk group was noted to have higher 100 day mortality and NRM compared to the low and high risk groups.
To our knowledge, this is first study to correlate pre-transplant HCT-CI with PACT scores in lymphoma pts who underwent ASCT. Higher HCT-CI was associated with lower socioeconomic status, poor mental health and coping skills, unhealthy lifestyle habits, decreased medical/transplant knowledge and compliance. HCT-CI did not predict survival in our cohort. Further studies are needed to investigate the association between psychosocial risk factors and HCT-CI and define their combined utility in pre-transplant risk assessment in ASCT patients.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.