Abstract
Objectives: In cancer patients undergoing intensive therapy such as stem cell transplant, functional recovery is an important but challenging outcome to measure. This prospective, longitudinal study aimed to demonstrate how a patient-reported outcome (PRO) could predict patient-performed testing (PPT) for measuring functional impairment after autologous stem cell transplant (ASCT) in patients with multiple myeloma (MM).
Methods: A secondary analysis was conducted using data from a randomized controlled trial of 2 stem cell doses for MM patients undergoing ASCT. Symptom interference on walking (a PRO) was measured by the MD Anderson Symptom Inventory (MDASI), on a 0-10 scale, with a higher score referring to a greater interference. The PPT outcome was assessed via distance walked on the six-minute walk test (6MWT). MDASI and 6MWT were administrated before ASCT, and on days 0, 3, 5, 7, 14, 21 and 28 from ASCT. Mixed effects modeling was used to examine 1) the longitudinal relationship between MDASI-walking symptom interference score and 6MWT walking distance and 2) the MDASI-walking symptom interference scores between patients who completed 6WMT and those who did complete the test.
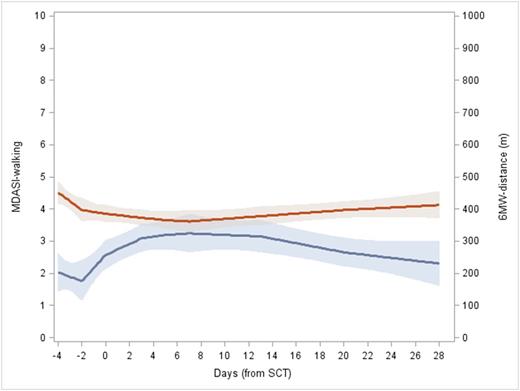
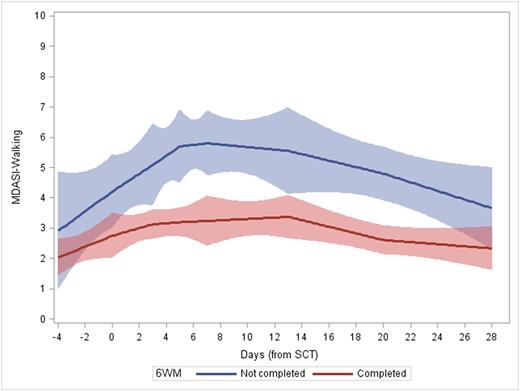
Results: Seventy-nine patients were included in the study. Of note, no significant clinical, functional or symptom differences were detected between the 2 doses of stem cells (Shah et al, BBMT 2015); thus the entire study population was considered in the same cohort. The average pre-ASCT walking distance was 452±185 feet and MDASI-walking score was 2.1±2.6. From day of transplant, the 6MWT decreased until day 5 (329±140, P=0.04, compared to pre-ASCT) and then recovered to pre-ASCT level at day 28 (408±131, p=0.176, compared to pre-ASCT). MDASI-walking interference symptom score worsened until day 7 (4.7±3.2, P<.0001, compared to pre-ASCT level) and returned to pre-ASCT level at day 28 (2.8±2.9, P=0.138). The 6MWT-walking distance significantly correlated with the MDASI-walking interference symptom score over the first month of ASCT (est=-6.09, p=0.006, Figure 1). All patients (79) completed pre-ASCT MDASI and 70 completed 6MWT pre-ASCT. Completion rate for both measures were decreased after ASCT. The lowest completion rate for 6MWT was found on day 7 (38%) and day 14 for MDASI (76%). There was a significantly higher completion rate for the MDASI versus 6MWT at each time point (p<0.01 for all). Patients who completed the 6MWT reported lower MDASI-walking scores (indicating better walking functioning) than those who did not complete 6MWT at day 3 (3.25 vs. 5.09, p=0.033), day 5 (3.09 vs. 5.70, p=0.02), day 7 (3.30 vs. 5.80, p=0.02), and day 14 (3.45 vs. 5.55, p=0.019). The mixed model showed that this difference was significant over the transplant course (est=1.61, p<.0001, Figure 2).
Conclusion: PRO-based functioning as measured by an interference item on the MDASI significantly correlates with a functional measure such as the 6MWT in MM patients undergoing ASCT. As patients with poorer functional status during ASCT are more likely to miss the 6MWT, the MDASI or other PRO tools may offer a more practical quantitative measure of functioning in patients with low functional status. This is one of the first studies to demonstrate a link between a PRO and objective physical functional status by a longitudinal study in ASCT.
MDASI-walking and 6MWT-walking distance are longitudinally correlated (est=-6.09, p=0.006)
MDASI-walking and 6MWT-walking distance are longitudinally correlated (est=-6.09, p=0.006)
MDASI-walking scores between patients completing or not completing 6MWT (est=1.61, p<.0001)
MDASI-walking scores between patients completing or not completing 6MWT (est=1.61, p<.0001)
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.