Abstract

Background: Chimeric antigen receptors (CARs) are fusion proteins that combine antigen-recognition domains and T-cell signaling domains. T cells genetically modified to express CARs directed against the B-cell antigen CD19 can cause remissions of B-cell malignancies. Most CARs in clinical use contain components derived from murine antibodies. Immune responses have been reported to eliminate CAR T cells in clinical trials, especially after second infusions of CAR T cells (C. Turtle et al., Journal of Clinical Investigation, 2016). These immune responses could be directed at the murine components of CARs. Such immune responses might limit the persistence of the CAR T cells, and anti-CAR immune responses might be an especially important problem if multiple infusions of CAR T cells are administered. Development of fully-human CARs could reduce recipient immune responses against CAR T cells.
Methods: We designed the first fully-human anti-CD19 CAR (HuCAR-19). The CAR is encoded by a lentiviral vector. This CAR has a fully-human single-chain variable fragment, hinge and transmembrane regions from CD8-alpha, a CD28 costimulatory domain, and a CD3-zeta T-cell activation domain. We conducted a phase I dose-escalation trial with a primary objective of investigating the safety of HuCAR-19 T cells and a secondary objective of assessing anti-lymphoma efficacy. Low-dose chemotherapy was administered before HuCAR-19 T-cell infusions to enhance CAR T-cell activity. The low-dose chemotherapy consisted of cyclophosphamide 300 mg/m2 daily for 3 days and fludarabine 30 mg/m2 daily for 3 days on the same days as cyclophosphamide. HuCAR-19 T cells were infused 2 days after the end of the chemotherapy regimen. Patients with residual lymphoma after a first treatment were potentially eligible for repeat treatments if dose-limiting toxicities did not occur with the first treatment. Repeat infusions were given at the same dose level as the first infusion or 1 dose level higher than the first infusion.
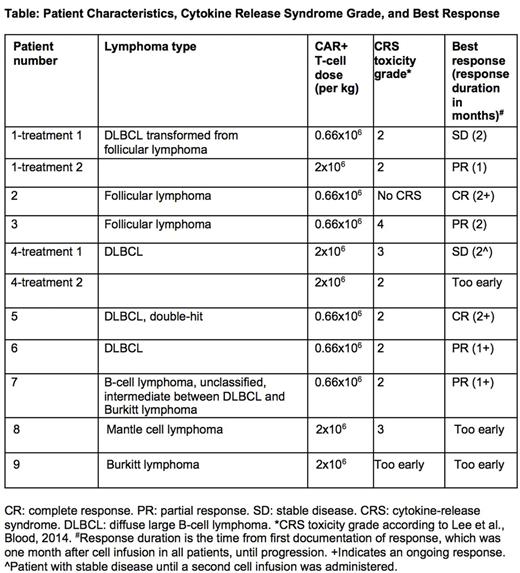
Findings: A total of 11 HuCAR-19 T-cell infusions have been administered to 9 patients; 2 patients received 2 infusions each. So far, there is an 86% overall response rate (Table). Grade 3 adverse events (AEs) included expected cytokine-release syndrome toxicities such as fever, tachycardia, and hypotension. Corticosteroids were used to treat toxicity in Patient 3. The interleukin-(IL)-6 receptor antagonist tocilizumab was used to treat toxicity in Patient 4, and both tocilizumab and corticosteroids were used to treat toxicity in Patient 8. Only 1 of 8 evaluable patients, Patient 3, has experienced significant neurological toxicity to date. This patient experienced encephalopathy that was associated with a cerebrospinal fluid (CSF) white blood cell count of 165/mm3. Almost all of the CSF white cells were CAR T cells, and the CSF IL-6 level was elevated. All toxicities have resolved fully in all patients.
In Patient 1, tumor biopsies revealed a complete loss of CD19 expression by lymphoma cells after 2 HuCAR-19 T-cell infusions, which to our knowledge is the first documented complete loss of CD19 expression by lymphoma after anti-CD19 CAR T-cell therapy. This loss of CD19 expression was associated with lymphoma progression.
After first CAR-19 T-cell infusions, HuCAR-19 cells were detectable in the blood of every patient. The median peak number of blood CAR+ cells was 26/microliter (range 3 to 1005 cells/microliter). Blood HuCAR-19 cells were detected after second infusions in the blood of both patients who received second infusions. Patient 1 obtained a partial response after a second infusion after only obtaining stable disease after a first infusion. We detected elevations of inflammatory cytokines including IL-6, interferon gamma, and IL-8 in the serum of patients experiencing clinical toxicities consistent with cytokine-release syndrome.
Interpretation: T cells expressing HuCAR-19 have substantial activity against advanced lymphoma, and infusions of HuCAR-19 T cells caused reversible toxicities attributable to cytokine-release syndrome.
Kochenderfer:Kite Pharma: Patents & Royalties, Research Funding; bluebird bio: Patents & Royalties, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract