Abstract
Heparin-induced thrombocytopenia (HIT) is an immune complication of heparin therapy caused by antibodies to complexes of platelet factor 4 (PF4) and heparin. Pathogenic antibodies to PF4/heparin bind and activate cellular FcγRIIA on platelets and monocytes to propagate a hypercoagulable state culminating in life-threatening thrombosis. It is now recognized that anti-PF4/heparin antibodies develop commonly after heparin exposure, but only a subset of sensitized patients progress to life-threatening complications of thrombocytopenia and thrombosis. Recent scientific developments have clarified mechanisms underlying PF4/heparin immunogenicity, disease susceptibility, and clinical manifestations of disease. Insights from clinical and laboratory findings have also been recently harnessed for disease prevention. This review will summarize our current understanding of HIT by reviewing pathogenesis, essential clinical and laboratory features, and management.
Introduction
Unfractionated heparin (UFH) celebrated its centennial from discovery in 2016.1 In recognizing this historical milestone, it is fitting to acknowledge heparin’s continued relevance to modern medicine. None of the newer anticoagulants, whether oral or parenteral, combine heparin’s unique pharmacologic properties, including a rapid onset of action, ability to inhibit multiple coagulant proteins, ease of monitoring, and reversibility. Such favorable properties will continue to keep UFH and its derivatives, the low-molecular-weight heparins (LMWHs), at the therapeutic forefront for a number of indications where alternative therapies are currently lacking (cardiac surgery), unsuitable (mechanical valves), or untested (cancer associated thrombosis and antiphospholipid antibody syndrome). Thus, as a drug class, the heparin family (UFH and LMWH) is likely to remain in clinical use for the foreseeable future.
Heparin-induced thrombocytopenia (HIT) is heparin’s most clinically relevant nonhemorrhagic complication. It is an immune complication caused by antibodies directed to complexes containing heparin and an endogenous platelet protein, platelet factor 4 (PF4). Although the immune reaction is common (8% to 50%),2-4 clinical complications of thrombocytopenia and thrombosis are far less frequent, affecting ∼0.2% to 3% of patients exposed to the drug in various clinical settings.2,5,6 This review will summarize our current understanding of the clinical syndrome from disease pathogenesis to its treatment.
Historical perspective
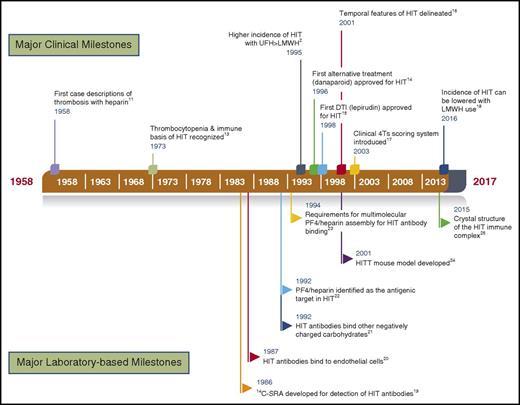
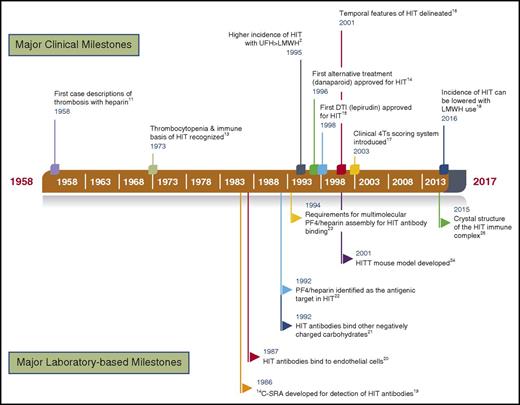
Acute thrombocytopenia occurring within minutes of heparin therapy was first described in animals in 19427 and later observed in humans8 as a transient, nonimmune complication of heparin therapy. This pharmacologic effect of heparin, referred to as type I HIT9 is caused by the agglutinating effects of heparin on platelets.10 The more serious, immune complication of HIT (type II) was first reported in 1958 by 2 surgeons, Weismann and Tobin, who summarized a case series of 10 patients at their institution who developed paradoxical thrombosis while receiving heparin therapy.11 Similar findings were noted a few years later by Roberts et al12 who described another case series of 11 patients and postulated that this clinical syndrome may be “the result of an antigen-antibody mechanism.” By 1973, Rhodes et al succinctly described salient clinical features of this disease through systematic investigation of 2 patients with HIT, noting the following: (1) concurrent manifestations of thrombocytopenia in addition to thrombosis during heparin therapy, (2) improvement in platelet counts after discontinuation of heparin therapy, (3) demonstration of a heparin-dependent antibody using platelet aggregation assays in the acute phase, and (4) recurrent thrombocytopenia with heparin rechallenge during the acute phase of illness.13 Since these initial descriptions, major clinical2,14-18 and laboratory19-25 discoveries over the ensuing decades have further refined our understanding of the disease. A time line of some of the landmark studies, in the opinion of the author, is provided in Figure 1. For a detailed historical perspective on HIT, the reader is referred to the excellent review by Kelton and Warkentin.26
A time line of key clinical and laboratory-based observations in HIT. Important clinical developments are provided above the time band, and major research observations are noted below. DTI, direct thrombin inhibitor; HITT, HIT with thrombosis; SRA, serotonin release assay.
A time line of key clinical and laboratory-based observations in HIT. Important clinical developments are provided above the time band, and major research observations are noted below. DTI, direct thrombin inhibitor; HITT, HIT with thrombosis; SRA, serotonin release assay.
Pathogenesis of HIT: antigen, antibody, and thrombotic mechanisms
HIT is caused by antibodies that recognize complexes of PF4 and heparin.22 Once antibodies form, a subset of patients develops a profound hypercoagulable state caused by cellular-activating antibodies that promote thrombin generation. This section summarizes our current understanding of the HIT antigen, triggers for PF4/heparin antibody formation, and mechanisms of thrombosis.
The HIT antigen: PF4/heparin complex
PF4 is a positively charged platelet protein stored in platelet α-granules and released in high quantities at sites of platelet activation.27 Released PF4 binds to negatively charged glycosaminoglycans (GAGs) on nearby endothelial cells, displaces bound antithrombin,28 and renders the local milieu prothrombotic. Because of the higher affinity of PF4 for heparin relative to other GAGs (heparin > heparan sulfate > dermatan sulfate > chondroitin 6-sulfate > chondroitin 4-sulfate),29 infusions of heparin displace released PF4 from vascular or other cell-binding sites into the circulation allowing for formation of immunogenic PF4/heparin complexes.
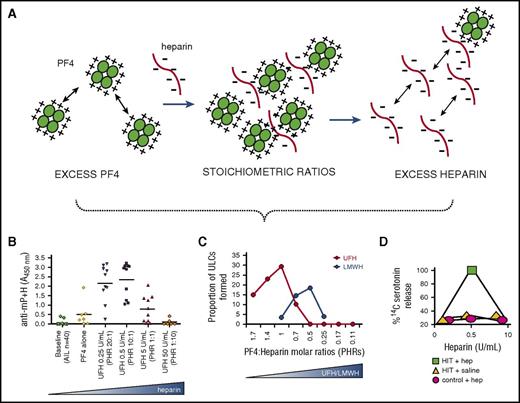
PF4 and heparin interactions are exclusively charge dependent.30 Optimal PF4/heparin complex formation occurs when the 2 compounds are present at certain molar amounts associated with charge neutralization.31-33 Changes in molar amounts of PF4 or heparin leading to excess of one component or another results in charge imbalance and increased repulsive forces that affect complex assembly. These fundamental chemical properties of PF4 and heparin result in the appearance of a “bell-shaped” curve of reactivity corresponding to heparin-dependent reactivity in laboratory assays,19,23 differences in complex formation between UFH and LMWH,31,34 and in vivo immunogenicity33 (Figure 2). Recent structural studies have additionally identified critical thermodynamic35,36 and essential structural features of the antigenic complex that govern chemical interactions.25
Importance of PF4/heparin ultralarge complexes (ULCs) in HIT pathogenesis. (A) PF4, a positively charged protein, binds to negatively charged heparin through electrostatic interactions to form ULCs that govern HIT biology. At concentrations of PF4 or heparin excess, repulsive forces from excess charge predominate and are not permissive for complex formation. At stoichiometric ratios associated with charge neutralization, ULCs form capable of biological effects associated with in vivo immunogenicity33 (B), differential clinical effects of UFH and LMWH31 (C), and heparin-dependent reactivity in laboratory assays19 (D).
Importance of PF4/heparin ultralarge complexes (ULCs) in HIT pathogenesis. (A) PF4, a positively charged protein, binds to negatively charged heparin through electrostatic interactions to form ULCs that govern HIT biology. At concentrations of PF4 or heparin excess, repulsive forces from excess charge predominate and are not permissive for complex formation. At stoichiometric ratios associated with charge neutralization, ULCs form capable of biological effects associated with in vivo immunogenicity33 (B), differential clinical effects of UFH and LMWH31 (C), and heparin-dependent reactivity in laboratory assays19 (D).
The HIT antibody
It is now recognized that the immune response to PF4/heparin occurs far more frequently than clinical manifestations of thrombocytopenia or thrombosis.6,37,38 The incidence of antibody formation in general medical and surgical patients treated with UFH is 8% to 17%,37 for LMWH and fondaparinux is 2% to 8%,6,39,40 and approaches ∼50% in patients undergoing cardiac surgery.4,38,41 Several theories have been advanced to explain this unusually high frequency of anti-PF4/heparin antibodies. PF4 binds effectively to bacterial walls of gram-positive and gram-negative bacteria,42-44 and bacterial infection, if accompanied by platelet activation and PF4 release, may provide a sufficient priming stimulus for an immune response upon subsequent heparin exposure.42
Our laboratory’s investigations have shown a more direct role for PF4/heparin complexes in dysregulating innate immunity.45 In vitro studies and ex vivo studies of heparinized patients demonstrate nearly exclusive binding of PF4/heparin complexes to B cells. Further evaluation revealed that B-cell binding is mediated by C3 activation by PF4/heparin ULCs and subsequent binding of complement-opsonized antigen to B cells via complement receptor 2/CD21.45 As binding of complement-coated antigen to CD21 enhances its immunogenicity by 1000- to 10 000-fold,46 it is likely that direct complement activation by PF4/heparin complexes45 contribute to subsequent antibody production. Other investigators have described findings of autoreactive B cells secreting anti-PF4/heparin immunoglobulin M (IgM) in human cord blood and peripheral blood of healthy subjects.44,47 These latter studies suggest that inflammation and/or infection transiently lift peripheral tolerance mechanisms to allow proliferation of autoreactive B cells.47,48
Mechanisms of HIT thrombosis
Once an immune response occurs, a subset of seropositive patients experience thrombocytopenia and progress to life-threatening complications of thrombosis. The principal cellular target for HIT antibodies is platelets, which express FcγRIIa receptors.49 These findings were confirmed in a murine model by Reilly et al, who demonstrated the requirements for anti- PF4/heparin antibodies and cellular FcγRIIA for disease manifestations.24 Binding of HIT antibodies to platelet FcγRIIA elicits platelet activation via intracellular signaling involving the spleen tyrosine kinase (Syk50 ) and release of procoagulant microparticles.51
Platelet activation in HIT is also accompanied by intense thrombin generation.52 The mechanisms underlying thrombin generation in HIT are not fully understood, but recent studies indicate that cellular activation of monocyte FcγRIIA promotes tissue factor expression, which in turn facilitates platelet activation via thrombin.53-55 Studies by Tutwiler et al recently provided experimental proof of this amplification loop.56 Using in vitro and in vivo studies, these investigators showed that HIT antibodies triggered dual activation of platelets and monocytes via cellular FcγRIIA. They further showed that depleting monocytes and/or blocking monocyte FcγRIIA diminished monocyte-derived thrombin, which provided a second signal for platelet activation via protease-activated receptor 1 (PAR-1).56 These findings further underscore the vital contributions of varied cellular FcγRIIA in HIT pathogenesis.
Epidemiology of HIT
Anti-PF4/heparin antibodies are extremely uncommon in healthy individuals (0.3% to 0.5%) as assessed in large studies of blood bank donors42,57 . Recent studies suggest that autoantibodies to PF4/heparin can develop in the context of surgical inflammation.40 In addition, infection and surgical inflammation can also give rise to “spontaneous HIT,” a rare clinical variant occurring without antecedent heparin exposure.58,59 In reports of spontaneous HIT, complications of unexplained thrombocytopenia and/or thrombosis are accompanied by laboratory evidence of high-titer platelet activating anti-PF4/heparin antibodies.58,59 Clinical and laboratory features of several case reports to date are summarized in Table 1.
The vast majority of patients with HIT, however, develop clinical disease in the wake of heparin exposure. The incidence of disease varies by clinical setting, heparin formulation (UFH vs LMWH), and to some extent, drug dose (prophylactic vs therapeutic). Adults receiving UFH or LMWH for medical or general surgical indications are at higher risk for HIT6 than pediatric60 or obstetric patients.61,62 These population differences are attributed to the existence of preexisting vascular disease and alterations in basal levels of platelet activation and circulating PF4. Other minor influences on HIT epidemiology have been described, including biological source of heparin (bovine > porcine63 ), route (intravenous > subcutaneous64 ), and sex (females > males).65
The differential immunogenicity and incidence of HIT with UFH and LMWH were first noted in a study by Warkentin et al in 1995.2 In this study of ∼700 orthopedic patients randomized to receive prophylactic dose UFH or LMWH, they noted a lower incidence of HIT (2.7% UFH vs 0% LMWH; P = .0018) and platelet activating antibodies (7.8% UFH vs 2.2% LMWH; P = .02).2 Subsequent studies and a meta-analysis of ∼7300 patients have confirmed nearly a 10-fold lower risk of HIT with use of prophylactic dose LMWH as compared with UFH.66 This differential effect, however, is not seen at therapeutic doses of UFH and LMWH. In a meta-analysis of studies using these drugs at therapeutic doses, the incidence of clinical HIT appeared to be comparable (UFH 1.5% vs LMWH 1.2%).67,68 Differences in the immunogenicity of prophylactic vs therapeutic doses of LMWH could potentially be explained by LMWH concentrations required to form immunogenic ULCs (Figure 2; see Rauova et al31 ).
The differential immunogenicity of prophylactic dose UFH and LMWH can be harnessed for disease prevention.18,69 Investigators at Sunnybrook Health Sciences Center in Toronto implemented an “Avoid Heparin” campaign where they systematically replaced UFH with LMWH for thromboprophylaxis and/or treatment and removed UFH from catheter flushes and nursing units. By doing so, investigators noted a dramatic reduction after implementation of this program with respect to suspected HIT (85.5 vs 49.0 cases per 10 000 admission; P < .001), positive HIT enzyme-linked immunosorbent assay (16.5 vs 6.1 cases per 10 000 admission; P < .001), and adjudicated cases of HIT/HITT (10.7/4.6 vs 2.2/0.4 cases per 10 000 admission; P < .001).18
Clinical features of HIT
The clinical diagnosis of HIT rests on demonstrating thrombocytopenia and/or thrombosis in temporal association with heparin therapy while excluding other causes of thrombocytopenia. Such an exercise is rarely straightforward in hospitalized patients who are often on heparin thromboprophylaxis5 and have competing causes of thrombocytopenia (infection, other medications, intravascular devices, and surgery).70,71 The following section will summarize the essential diagnostic features of HIT (thrombocytopenia, thrombosis, and temporal features) and discuss clinical scoring systems that have been developed to assist clinicians in disease risk stratification.
Thrombocytopenia
The cardinal manifestation of HIT is the occurrence of thrombocytopenia, which occurs in ∼95% patients in temporal association with heparin therapy.72 Thrombocytopenia can manifest either as an absolute drop in platelet count (<150 × 109/L) or a relative decline of 30% to 50% from baseline platelet counts.72 Absolute thrombocytopenia in HIT is often moderate (50-70 × 109/L) and typically not associated with bleeding complications. Severe thrombocytopenia (<20 × 109/L) can occur as a manifestation of fulminant thrombotic disease72 and consumptive coagulopathy.73 Patients who only manifest an isolated thrombocytopenia (isolated HIT) remain at high risk for subsequent thrombosis (20% to 50%) from circulating antibodies capable of binding endogenous PF4/GAG complexes.74,75 With unusual presentations of HIT, such as heparin-induced skin necrosis, thrombotic complications can occur in the absence of thrombocytopenia.76
Thrombosis
Thrombosis is the most severe complication of HIT and contributes to disease morbidity and mortality.64,75 In most patients, thrombotic complications occur concurrently with thrombocytopenia72 and can affect any vascular bed. Venous thromboses predominate, particularly at sites of vascular injury from catheters.77 Atypical presentations, such as bilateral adrenal hemorrhage,78 venous limb gangrene, and skin necrosis should prompt diagnostic consideration of HIT.76
Presently, it is not known why some seropositive patients remain asymptomatic while others progress to severe disease. There are no differences in traditional thrombophilic markers such as protein C, protein S, antithrombin, or factor V Leiden.79,80 Although several studies have shown no major role for the common platelet FcγRIIA polymorphisms (FcγRIIAH131R)81 and risk for HIT, one recent study challenges these earlier observations based on new biological findings. These investigators noted a higher risk of thrombosis in individuals homozygous for the 131-RR genotype82 because of the inability of endogenous monomeric IgG2 (which binds the H-, but not the R-isoform) to effectively compete with HIT immune complexes for binding platelet FcγRIIA.82
Clinical studies indicate that certain serologic features, such as IgG isotype,83 capacity to activate platelets,84 and high antibody levels (as measured by optical density [OD] and/or titer84-86 ) are associated with thrombotic risk. The contribution of IgA or IgM isotypes to thrombosis in HIT87,88 is likely subordinate to established pathogenic mechanisms directly linking IgG-mediated activation of platelet and monocyte FcγRIIa receptors to thrombin generation.24,56 Severity of thrombocytopenia serves as another clinical correlate of thrombotic risk, as patients with marked thrombocytopenia (>90% decline from baseline counts) have greater than eightfold risk of thrombosis as compared with patients with <30% decline.72
Temporal features
The most important diagnostic element of HIT is timing of complications relative to heparin therapy. In heparin-naïve individuals, PF4/heparin antibodies become detectable at a median of 4 days from start of heparin therapy.89 Clinical manifestations of thrombocytopenia and/or thrombosis develop 5 to 14 days after initial heparin therapy,72,89 and on average ∼2 days (range 1-5 days) after antibody detection.89 In patients with recent heparin exposure (<100 days), thrombocytopenia occurs precipitously within 24 hours of drug reexposure because of circulating anti-PF4/heparin antibodies. Another rare clinical variant called “delayed-onset HIT” is recognized days to weeks after heparin discontinuation. Although thrombocytopenia likely occurs in the expected time frame after heparin exposure, there is a delay in manifestations of thrombosis days to weeks after discharge. If unrecognized, patients may be inadvertently reexposed to heparin leading to significant morbidity and mortality.90,91 Delayed-onset HIT is caused by antibodies that are cross-reactive with PF4/GAG complexes found on cell surfaces and can trigger heparin-independent platelet activation in functional assays.90
The median time to antibody clearance is 50 days for platelet activation assays and 85 to 90 days by immunoassays.16,92 Immunoassays may remain positive in ∼35% of patients for up to 1 year, with levels decreasing over time.92 Platelets rebound to the normal range within 1 week of discontinuation in ∼65% of patients.93 Even with platelet count recovery, patients remain at risk for thrombosis for 4 to 6 weeks after diagnosis74 because of circulating anti-PF4/heparin antibodies.16 Presently, there is no compelling laboratory or clinical evidence for immunologic memory in patients with HIT.16,94-96 Patients who are reexposed to the drug months to years after antibody disappearance often do not manifest anamnestic responses, and seroconversion risk appears similar to de novo heparin exposure.16,95,96 In a small study of 17 patients with HIT who are reexposed to heparin for cardiac surgery, a higher proportion of patients developed anti-PF4/heparin antibodies (65%) relative to the incidence described in the literature (∼27% to 51%).4,38,41,97
Clinical scoring systems
Clinical scoring tools have been developed to aid clinicians in ascertaining disease. The 4Ts clinical scoring system, developed by Warkentin is the simplest and most widely used risk assessment tool for HIT.98-101 The 4Ts incorporates essential features of disease described previously (timing of heparin therapy, complications of thrombocytopenia and thrombosis, and exclusion of other causes) and categorizes disease likelihood based on the cumulative score (low risk: 0-3; intermediate risk: 4-5; high risk: 6-8). A recent meta-analysis of studies confirmed that the clinical utility of the 4Ts is the greatest for excluding HIT. A low 4Ts score (≤3) carries a high negative predictive value (0.998; 95% confidence interval, 0.970-1.000).99 Intermediate (4Ts: 4-5) and high (4Ts: >6) scores on the other hand performed poorly in predicting disease because of significant inter-operator variability.99 A recent prospective study utilizing the 4Ts suggests that assignment of low 4T scores can also be subject to operator inexperience, resulting in misclassification in ∼2% of cases.101
The HIT expert probability score is another clinical scoring system developed by Cuker and colleagues utilizing 8 clinical features and broad expert opinion to assign clinical significance.102 In initial descriptions, when compared with the 4Ts score, the HIT expert probability score demonstrated improved correlation with serologic HIT testing and improved inter-observer agreement.102 This scoring system is currently undergoing prospective validation.
Laboratory diagnosis of HIT
A diagnosis of HIT cannot be made without laboratory evidence of anti-PF4/heparin antibodies. Laboratory assays detect the presence of HIT antibodies using platelet activation assays (“functional”) or by immunoassays. Platelet activation assays, such as the 14C-SRA,19 platelet aggregation,103 and more recent flow-based platelet activation assays104,105 detect antibodies capable of binding and cross-linking platelet FcγRIIA. In stringently defined cases of HIT, the functional assays offer high specificity (>95%)39 and PPVs (89% to 100%) but lower sensitivity (56% to 100%).39,106 The reduced sensitivity of assays depends on the functional end points of the assay (light transmission < flow based < radioactive signals). The functional assays are technically more challenging and thus not routinely performed at most medical centers.
Immunoassays, on the other hand, measure the presence of anti-PF4/heparin antibodies using a variety of antibody capture platforms (enzyme-linked immunosorbent assay, particle gel, immunoturbidimetric etc.). For detailed information on performance characteristics of HIT immunoassays, the reader is referred to recent comprehensive reviews on this topic.107,108 Advantages of immunoassays are technical simplicity and high sensitivity (>99%). However, immunoassays lack specificity (30% to 70%) for the diagnosis of HIT109 because of the occurrence of asymptomatic seroconversions. Specificity of immunoassays can be increased through detection of IgG antibodies and numerical quantification of OD and/or titers. A number of studies have shown increased correlation between high ODs with platelet activating antibodies, clinical HIT and thrombotic risk.86,110
For most patients suspected of HIT (high or intermediate 4Ts), combining clinical scoring data with immunoassay results offers greater diagnostic utility than either approach alone and often, can bypass the need for functional assays. Retrospective111 and prospective studies101,112 have shown that for patients with a high clinical suspicion of HIT by the 4Ts (eg, >6), whose immunoassays confirm anti-PF4/heparin antibodies, the likelihood of positive functional assays is sufficiently high (83% to 95%) that additional platelet activation assays become unnecessary. For patients in the “intermediate” category (4Ts = 4-5) of clinical suspicion for HIT, a negative immunoassay virtually eliminates the possibility of HIT reducing pretest probabilities from 7% to 14% to posttest probabilities of ∼0% to 0.4%.111 A positive immunoassay for the intermediate risk group, however, increases the posttest probability of HIT to 40% to 64%.111 It is in this category of patients where additional functional assays may be informative.
Treatment of HIT
Management of HIT begins at time of disease suspicion, and includes discontinuation of all sources of heparin and administration of one of the parenteral alternative agents described subsequently. Selection of a parenteral agent is largely based on drug availability and patient cm-morbidities (renal or hepatic dysfunction). In the United States, intravenous direct thrombin inhibitors are preferred agents in the critically ill population who often require multiple procedures and may be at higher bleeding risk. Overlap with a vitamin K antagonist (VKA) should be initiated only after platelet counts recover to a stable baseline or greater than 150 × 109/L.113 Initiation of VKA prior to platelet count recovery is contraindicated because of heightened risk for venous limb gangrene from the combined effects of VKA and anti-PF4/heparin antibodies on protein C reduction.114,115 Additionally, if a patient is being treated with a VKA at time of diagnosis, reversal with vitamin K is recommended to lower the risk of venous limb gangrene and warfarin-induced skin necrosis.113
Duration of anticoagulation therapy for HIT is based on concurrence of thrombosis. American and British guidelines recommend therapeutic dose anticoagulation for 4 weeks in patients with isolated HIT and 3 months for HIT patients with thrombosis.113,116 Prospective data are lacking on the best approach for managing future heparin exposure in patients with a confirmed diagnosis of HIT. Guidelines recommend limiting heparin reexposure in patients with a prior history of HIT, except in seronegative patients who require cardiac surgery.113,116 For a more comprehensive discussion on the management of patients with a prior history of HIT, the reader is referred to a recent review by Warkentin on this topic.59
Parenteral anticoagulants
Danaparoid is a mixture of naturally occurring GAGs (heparan sulfate, dermatan, and chondroitin) sulfate and was the first alternative agent available for the treatment of HIT. Although the drug has not been available in the US market since 2002, it is currently approved in several countries outside the United States (Europe, Canada, Japan, and Australia) for treatment of HIT. It is the only agent that has been compared with an alternative agent (dextran 70) in a prospective randomized trial.118 Fifty-six percent of patients treated with danaparoid experienced complete clinical recovery from thromboembolic events as compared with 14% randomized to dextran 70 treatment (P = .02).118
Argatroban, a small, synthetic reversible inhibitor of thrombin, is approved for treatment of HIT (argatroban) based on 2 multicenter trials comparing argatroban with historical controls. In these studies of HIT patients with and without thrombosis, argatroban therapy resulted in a reduced composite end point of death, amputation, and thrombosis (26% to 44.0%) as compared with historical controls (39% to 56%).75,119 Argatroban is hepatically cleared, and dose reductions are essential in patients with liver disease or who are critically ill with multiorgan failure. Argatroban dosing nomograms have been developed for use in special intensive care unit populations.120 Argatroban prolongs the prothrombin time at therapeutic doses, which must be taken into consideration at time of transition to warfarin therapy.
Bivalirudin is also a synthetic thrombin inhibitor that is cleared by plasma proteases and partially cleared by renal excretion. Bivalirudin is approved in the United States for patients who are undergoing percutaneous cardiac intervention and who either have HIT or are at risk for developing HIT. Although medical treatment of HIT is not a US Food and Drug Administration–approved indication, bivalirudin is routinely used for this purpose in the United States. Bivalirudin prolongs the prothrombin time, but to a lesser extent than argatroban.
Fondaparinux, a synthetic pentasaccharide LMWH121 is another anticoagulant that is being increasingly used off-label for the management of HIT.122 Fondaparinux does not cross-react with HIT antibodies, but has been rarely implicated as a cause of HIT in case reports.123 In a retrospective study of 133 patients receiving fondaparinux for HIT, thrombosis and/or bleeding complications, however, did not significantly differ from propensity matched controls on DTI.124 Some case series document increased bleeding rates (∼10% to 22%) with this agent125,126 and its use must be carefully monitored in patients with renal compromise.
Emerging therapies
Direct oral anticoagulants (DOACs): Only a few case reports and/or case series have reported on the safety and efficacy of several DOACs in HIT. Rivaroxaban was studied in a small multicenter single arm prospective study, which was closed early because of poor enrollment127 In this small cohort of 22 HIT patients, rivaroxaban appeared to be safe and effective without occurrence of new thrombosis. In another case series, a heterogeneous group of 11 patients with HIT were treated with rivaroxaban, apixaban, or dabigatran. In these patients, there were no recurrent arterial or venous thrombosis or bleeding complications.128 Presently, there is insufficient clinical information to recommend use of DOACs in the management of HIT.
Conclusion
HIT remains a commonly encountered iatrogenic complication of heparin therapy in hospitalized patients. In the nearly 6 decades since the initial descriptions of the disease, there have been major advances in understanding the pathogenesis of HIT, its varied clinical complications and treatment. Emerging anticoagulant therapies hold promise not only for the treatment of HIT but also in reducing its incidence.
Acknowledgment
This work was supported by the National Institutes of Health, National Heart, Lung, and Blood Institute (grant P01 HL110860) (G.M.A.).
Authorship
Contribution: G.M.A. is the sole author of this manuscript.
Conflict-of-interest disclosure: G.M.A. is a consultant for makers of generic low-molecular-weight heparins (Momenta, Apotex) and receives royalties from the University of New Mexico, Science and Technology Corporation for exclusive licensing of the monoclonal antibody KKO.
Correspondence: Gowthami M. Arepally, DUMC Box 3486, Room 356A Sands Building, Duke University Medical Center, Durham, NC 27710; e-mail: arepa001@mc.duke.edu.