Key Points
CD27 expression on malignant B cells triggers CD70 reverse signaling in NK cells and improves lymphoma immunosurveillance.
CD70 reverse signaling in NK cells is mediated via the AKT signaling pathway and enhances survival and effector function.
Abstract
The interaction of the tumor necrosis factor receptor (TNFR) CD27 with its ligand CD70 is an emerging target to treat cancer. CD27 signaling provides costimulatory signals to cytotoxic T cells but also increases the frequency of regulatory T cells. Similar to other TNFR ligands, CD70 has been shown to initiate intracellular signaling pathways (CD70 reverse signaling). CD27 is expressed on a majority of B-cell non–Hodgkin lymphoma, but its role in the immune control of lymphoma and leukemia is unknown. We therefore generated a cytoplasmic deletion mutant of CD27 (CD27-trunc) to study the role of CD70 reverse signaling in the immunosurveillance of B-cell malignancies in vivo. Expression of CD27-trunc on malignant cells increased the number of tumor-infiltrating interferon γ–producing natural killer (NK) cells. In contrast, the antitumoral T-cell response remained largely unchanged. CD70 reverse signaling in NK cells was mediated via the AKT signaling pathway and increased NK cell survival and effector function. The improved immune control by activated NK cells prolonged survival of CD27-trunc–expressing lymphoma-bearing mice. Finally, CD70 reverse signaling enhanced survival and effector function of human NK cells in a B-cell acute lymphoblastic leukemia xenotransplants model. Therefore, CD70 reverse signaling in NK cells contributes to the immune control of CD27-expressing B-cell lymphoma and leukemia.
Introduction
CD27 is a member of the tumor necrosis factor receptor (TNFR) family that is expressed on T, B, and natural killer (NK) cells. CD27 signaling on lymphocytes leads, in conjunction with T-cell receptor–mediated signals, to improved proliferation, differentiation, and effector function.1-5 In humans, the expression of CD27 defines B-cell developmental stages. Naive B cells are CD27-negative, whereas memory B cells with somatically mutated immunoglobulin genes are CD27-positive.6 CD27 signaling on B cells enhances immunoglobulin production and promotes plasma cell differentiation.7 Although malignant lymphoma may develop from different stages of B-cell development, CD27 is expressed on nearly all non–Hodgkin lymphoma (NHL) of pre- and postgerminal center origin and on B-cell acute lymphoblastic leukemia (ALL).8-10 However, the expression varies considerably in follicular lymphoma and in diffuse large B-cell lymphoma (DLBCL). Interestingly, the expression of CD27 differs in subsets of DLBCL with high expression in the germinal-center–like subtype and low expression in the activated B-cell–like subtype.11 After ligation of CD27 with its unique ligand CD70,12 a soluble form of CD27 (sCD27) is released to the sera, and the level of sCD27 correlates with lymphoma load.8,13 High sCD27 levels are associated with poor outcome in patients with DLBCL.14
CD27 signaling is regulated by the expression of its unique ligand CD70. During immune activation, CD70 is transiently expressed on lymphocytes, NK cells, and subsets of dendritic cells.15-18 Aberrant expression of CD70 leads to increased secretion of inflammatory cytokines and immune dysfunction.19-21 In addition, CD70 is expressed on some lymphomas22-25 and solid tumors,26-31 where it correlates with poor prognosis.32,33
The role of the CD70/CD27 interaction in B-cell neoplasms remains ill defined. The cytoplasmic domain of CD27 binds to TNFR-associated factor 2 (TRAF2), which signals downstream via mitogen-activated protein kinase family proteins, leading to nuclear factor of κ light polypeptide gene enhancer in B-cells inhibitor, α degradation and nuclear factor “κ-light-chain–enhancer” of activated B cells activation.34 TRAF2 can also activate c-Jun N-terminal kinases family members, bind to the inhibitor of apoptosis proteins, and lead to upregulation of B-cell lymphoma-extra-large.2,35 Thus, ligation of CD27 with stimulating monoclonal antibodies (mAb) in vitro leads to expansion of lymphoma cells.36 In addition, similarly to other TNFR ligands, CD70 has an intrinsic signaling activity (CD70 reverse signaling). CD70 reverse signaling activates phosphatidylinositide 3-kinase and MAPK pathways that trigger the expansion of CD70-transgenic CD27-deficient B cells while inhibiting cell differentiation in vivo.37 CD70 antibodies induce the expansion of B-cell leukemia cells,25 NK and T-cell lymphoma cells,38 and enhance the effector functions of human T, NK, and Tγδ cell clones in vitro.39,40
The role of CD70 reverse signaling in cancer, especially in lymphoma development, remains unknown. We generated a cytoplasmic deletion mutant of CD27 (CD27-trunc) lacking the intracellular signaling domain and therefore the possibility to transmit CD27 forward signaling. Here, we document that CD27-trunc–expressing tumor cells induce the activation and expansion of CD70-expressing NK cells in vivo. Activated NK cells contribute to cancer immunosurveillance (ie, mice bearing CD27-expressing tumors survived significantly longer than mice with control tumors). Importantly, CD70 reverse signaling similarly increased survival and effector function of human NK cells in a B-cell ALL xenotransplant model. Our experimental data are supported by a gene expression analysis of Cd27 in a publicly available microarray dataset of patients with high-grade lymphoma. Patients with CD27high-expressing lymphoma survived significantly longer than patients with CD27low-expressing lymphoma.
Materials and methods
Patient samples and xenograft model
Cryopreserved bone marrow aspirates from patients enrolled in the ALL-BFM 2000 study were used. Informed consent was given in accordance with the declaration of Helsinki, and approval was granted by the Ethics Commission of the Canton Zurich (approval number 2014-0383). For in vivo experiments, 5 × 106 fluorescence-activated cell sorter (FACS)-sorted CD27+CD70− primary common B-cell ALL cells were injected IV into NSG mice.41 Following detection of 5% to 10% engraftment in the blood of recipient mice (week 4), 5 × 106 sorted CD27− human allogenic NK cells were injected IV. NK cells were purified from peripheral blood mononuclear cells of healthy donors using the MACS human NK cell isolation kit, from Miltenyi Biotec. Human NK cells were isolated from the spleen of ALL xenotransplanted mice 2 days after transfer for functional analysis.
Tumor and lymphoma induction
Fibrosarcoma tumors were induced as described in Matter et al.42 Briefly, 2 × 106 MC57 cells were injected subcutaneously (SC) into the flanks of RAG−/− mice. After 14 days, 1- to 2-mm3 tumor fragments were transplanted into flanks of recipient mice. For lymphoma induction, 1.5 × 106 Q2A lymphoma cells were injected SC into recipient mice. Alternatively, 1 × 105 Q2A cells were injected IV. Tumor volume of SC tumors was calculated using the formula V = π × abc/6, where a, b, and c are orthogonal diameters that were measured by a caliper at different time points.
Statistical analysis
Data are represented as mean ± standard error of the mean (SEM). Data were analyzed using 1-way analysis of variance (ANOVA) and Tukey’s multiple comparison test, Student t test (2-tailed), 1-sample t test, or 2-way ANOVA and Bonferroni post hoc test (P value shows interaction). Significance of differences in Kaplan-Meier survival curves was determined using the log-rank test (2-tailed). Spearman’s rank analysis was performed to study the significance of 2 variables’ correlation. P < .05 was considered significant; *P < .05; **P < .01; ***P < .001; n.s., not significant (P > .05).
Results
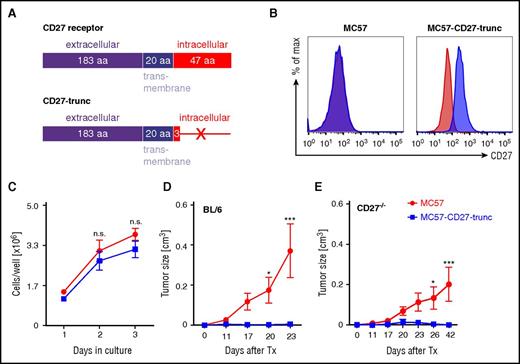
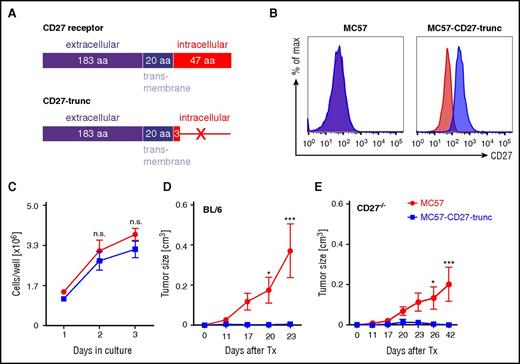
Expression of CD27-trunc on fibrosarcoma cells leads to tumor rejection
In contrast to hematological tumors, CD27 expression has not been documented on solid tumors so far.29,30 Therefore, in order to study CD70 reverse signaling in vivo, we transfected the fibrosarcoma cell line MC57 with a Cd27-trunc–expressing vector. The fibrosarcoma model provides a well-controlled system to dissect CD70 reverse signaling in these initial experiments, because it expresses neither CD27 nor CD70. The extracellular domain of the CD27-trunc receptor serves as the ligand for CD70 expressed on immune cells in the tumor microenvironment. However, CD27 forward signaling in MC57 is abrogated due to the excision of the intracellular C-domain (Figure 1A). Flow cytometric analysis revealed that the extracellular domain of CD27 was clearly detectable on MC57-CD27-trunc cells but not on parental MC57 cells (Figure 1B). MC57 and MC57-CD27-trunc cells did not express CD70 (supplemental Figure 1A, available on the Blood Web site). Transfection with Cd27-trunc did not alter the growth characteristic, and both cell lines showed a comparable expansion in vitro (Figure 1C).
Expression of CD27-trunc on MC57 fibrosarcoma promotes tumor rejection. (A) The amino acid sequences corresponding to CD27 receptor (top) or CD27-trunc (bottom) are shown. (B) Expression of CD27 on MC57 and MC57-CD27-trunc cells, analyzed by flow cytometry (1 representative experiment out of 3 is shown). Red: isotype; blue: CD27. (C) Growth curves of MC57 and MC57-CD27-trunc cells in vitro. Cells (0.5 × 106) were cultured in triplicate and counted on the days indicated. Total number of cells per well are shown. Results are representative of 3 independent experiments. (D-E) Tumor growth curves of MC57 and MC57-CD27-trunc tumors. MC57 and MC57-CD27-trunc tumor fragments were transplanted SC into the flanks of BL/6 (D) or CD27−/− mice (E) and tumor growth was monitored at the time points indicated. Data are shown as mean ± SEM of 5 to 10 mice in each group. Pooled data from 3 independent experiments are shown. Statistics: 2-way ANOVA (C-E). aa, amino acid; max, maximum; n.s., not significant; Tx, transplantation.
Expression of CD27-trunc on MC57 fibrosarcoma promotes tumor rejection. (A) The amino acid sequences corresponding to CD27 receptor (top) or CD27-trunc (bottom) are shown. (B) Expression of CD27 on MC57 and MC57-CD27-trunc cells, analyzed by flow cytometry (1 representative experiment out of 3 is shown). Red: isotype; blue: CD27. (C) Growth curves of MC57 and MC57-CD27-trunc cells in vitro. Cells (0.5 × 106) were cultured in triplicate and counted on the days indicated. Total number of cells per well are shown. Results are representative of 3 independent experiments. (D-E) Tumor growth curves of MC57 and MC57-CD27-trunc tumors. MC57 and MC57-CD27-trunc tumor fragments were transplanted SC into the flanks of BL/6 (D) or CD27−/− mice (E) and tumor growth was monitored at the time points indicated. Data are shown as mean ± SEM of 5 to 10 mice in each group. Pooled data from 3 independent experiments are shown. Statistics: 2-way ANOVA (C-E). aa, amino acid; max, maximum; n.s., not significant; Tx, transplantation.
Surprisingly, MC57-CD27-trunc tumors did not grow in vivo, whereas MC57 tumors developed large tumors within 3 weeks (Figure 1D). The expression of CD27-trunc on MC57-CD27-trunc tumors was confirmed by FACS analysis before transplantation (supplemental Figure 1B). Similarly to BL/6-recipient mice, MC57-CD27-trunc tumors were rejected in CD27−/− mice, whereas MC57 control tumors grew (Figure 1E). Rejection of MC57-CD27-trunc tumors in CD27−/− mice excludes that CD27-trunc expressed on tumor cells alters CD27 forward signaling on host immune cells due to excessive binding of the ligand. As documented before, due to lower numbers of regulatory T cells, tumor growth in CD27−/− mice was slower than in BL/6 mice.43 These data suggest that triggering CD70 reverse signaling in the tumor microenvironment leads to tumor rejection.
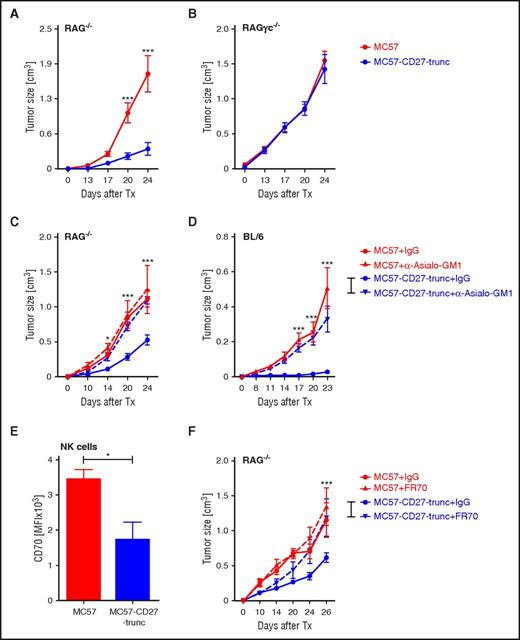
NK cells control CD27-trunc expressing tumors
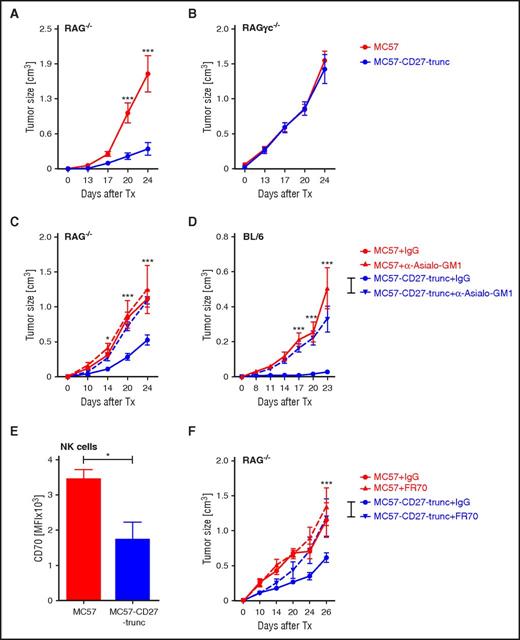
MC57 tumor cells are mainly controlled by CD8+ T cells.44,45 To analyze whether CD27-trunc activates CD70-expressing T cells leading to tumor rejection, MC57 and MC57-CD27-trunc tumor fragments were transplanted into RAG−/− mice, which lack mature NKT, B, and T lymphocytes. In line with previous findings,45 growth of transplanted MC57 tumor fragments in RAG−/− mice was substantially faster than in BL/6 mice (Figure 2A vs Figure 1D). However, MC57-CD27-trunc tumors developed substantially slower than control tumors independent of the adaptive immune system (Figure 2A).
CD70 reverse signaling in NK cells improves tumor control. (A-F) MC57 and MC57-CD27-trunc tumor fragments were transplanted SC into the flanks of RAG−/− (A,C,F), RAGγc−/− (B), and BL/6 (D) mice. Mice were treated with anti–Asialo-GM1 or control-IgG (C-D) or with FR70 or control IgG (F) at days −1, 0, and every second day after tumor transplantation. Tumor size was measured at the time points indicated. Data are shown as mean ± SEM of 5 to 10 mice in each group; representative of 3 independent experiments. (E) CD70 expression on tumor infiltrating NK cells from 3 tumor-bearing mice in each group at day 20 after transplantation. Histogram shows MFI of CD70 measured by FACS, representative of 3 independent experiments. Statistics: 2-way ANOVA (A-D,F), Student t test (E).
CD70 reverse signaling in NK cells improves tumor control. (A-F) MC57 and MC57-CD27-trunc tumor fragments were transplanted SC into the flanks of RAG−/− (A,C,F), RAGγc−/− (B), and BL/6 (D) mice. Mice were treated with anti–Asialo-GM1 or control-IgG (C-D) or with FR70 or control IgG (F) at days −1, 0, and every second day after tumor transplantation. Tumor size was measured at the time points indicated. Data are shown as mean ± SEM of 5 to 10 mice in each group; representative of 3 independent experiments. (E) CD70 expression on tumor infiltrating NK cells from 3 tumor-bearing mice in each group at day 20 after transplantation. Histogram shows MFI of CD70 measured by FACS, representative of 3 independent experiments. Statistics: 2-way ANOVA (A-D,F), Student t test (E).
RAG−/− mice have functional and highly activated NK cells46 that may contribute to the tumor control of MC57-CD27-trunc tumors. To test this, we transplanted MC57 and MC57-CD27-trunc tumors to RAGγc−/− mice that are deficient in T, B, and NK cells. Indeed, in the absence of NK cells, MC57-CD27-trunc tumors grew similarly to MC57 tumors (Figure 2B). Furthermore, NK cell depletion with anti–Asialo-ganglio-N-tetraosylceramide (GM1) antibody treatment restored tumor growth of MC57-CD27-trunc tumors to the growth of MC57 tumors in RAG−/− mice (Figure 2C). Similarly, depleting NK cells in BL/6 mice restored the growth of MC57-CD27-trunc to that of MC57 control tumors (Figure 2D). In contrast, anti–Asialo-GM1 treatment did not change growth of MC57 tumor fragments (Figure 2C), indicating that NK cells are not involved in tumor control in the absence of CD27-trunc expression. Importantly, MC57 and MC57-CD27-trunc similarly expressed inhibitory (major histocompatibility complex class I [MHC-I]; Qa-1B) and activating (MULT-1; Rae-1) NK cell ligands (supplemental Figure 1C).
CD70 is expressed on NK cells upon activation, and binding of CD70 to its receptor CD27 results in the downregulation of CD70 expression.47 Tumor-infiltrating NK cells in both MC57 and MC57-CD27-trunc tumors expressed CD70 (supplemental Figure 1D). However, the mean fluorescence intensity (MFI) of CD70 was significantly lower on NK cells from MC57-CD27-trunc tumors (Figure 2E), indicating that CD70 is ligated on NK cells in the tumor.
To analyze the role of CD70 signaling in NK cells in tumor development, we treated MC57 and MC57-CD27-trunc tumor-bearing mice with a blocking anti-CD70 mAb (FR70). Blocking the CD70/CD27 interaction in vivo in Rag1−/− mice did not affect tumor growth of the parenteral MC57 cells but restored the growth of MC57-CD27-trunc tumors to the level of control MC57 tumors (Figure 2F). In summary, these experiments indicate that the expression of CD27-trunc on tumor cells leads to the activation of NK cells by CD70 reverse signaling.
CD70 reverse signaling increases the frequency and function of tumor-infiltrating NK cells
We next analyzed the antitumoral immune response in BL/6 and RAG−/− recipient mice 12 days after tumor transplantation, at a time point when the MC57- and MC57-CD27-trunc tumor size was still comparable (supplemental Figure 2A). CD3+ T-cell number and interferon γ (IFN-γ) production after restimulation with phorbol 12-myristate 13-acetate (PMA)/ionomycin were comparable in spleens and draining lymph nodes (dLNs) (supplemental Figure 2B-D). Similarly, NK cell frequencies and numbers in spleens (Figure 3A) and dLNs (supplemental Figure 2E) were comparable. In addition, NK cells from spleen and dLNs similarly produced IFN-γ upon restimulation with PMA/ionomycin in vitro (supplemental Figure 2F-G). However, there was a significant increase in numbers of tumor-infiltrating NK cells in MC57-CD27-trunc tumor-bearing BL/6 and Rag−/− mice (Figure 3B; supplemental Figure 2H). Functionally, significantly more tumor-infiltrating NK cells in CD27-trunc expressing tumors produced INF-γ after restimulation in vitro (Figure 3C-E). Furthermore, individual NK cells produced more IFN-γ as demonstrated by a higher MFI of the IFN-γ staining in NK cells isolated from MC57-CD27-trunc tumors as compared with controls (Figure 3F). Together, these results indicate that CD27-trunc expression on tumor cells increases the numbers and the function of tumor-infiltrating NK cells.
CD27-trunc enhances the activity of tumor-infiltrating NK cells. (A-F) Analysis of NK cells in spleens (A) and tumor tissue (B-F) of MC57 or MC57-CD27-trunc tumor-bearing mice, 12 days after tumor transplantation. (A) Frequencies and numbers of NK cells in spleens of BL/6 mice. (B) Numbers of tumor-infiltrating NK cells. (C-F) MACS-sorted CD45+ cells from tumor tissue were restimulated with PMA/ionomycin for 4 hours and IFN-γ was analyzed by FACS. (C) One representative FACS plot of IFN-γ+ NK cells out of 3 is shown. (D) Frequencies of IFN-γ+ NK cells in tumor are shown as Δ (PMA/Iono-unstimulated). (E) Numbers of tumor-infiltrating IFN-γ+ NK cells. (F) Δ MFI, [MFI-stimulated – MFI-unstimulated], of IFN-γ expression in tumor-infiltrating NK cells. Data are shown as mean ± SEM of 3 to 5 mice in each group and are representative of 3 independent experiments. Statistics: Student t test (A-B,D-F). lono, ionomycin; SSC, side scatter.
CD27-trunc enhances the activity of tumor-infiltrating NK cells. (A-F) Analysis of NK cells in spleens (A) and tumor tissue (B-F) of MC57 or MC57-CD27-trunc tumor-bearing mice, 12 days after tumor transplantation. (A) Frequencies and numbers of NK cells in spleens of BL/6 mice. (B) Numbers of tumor-infiltrating NK cells. (C-F) MACS-sorted CD45+ cells from tumor tissue were restimulated with PMA/ionomycin for 4 hours and IFN-γ was analyzed by FACS. (C) One representative FACS plot of IFN-γ+ NK cells out of 3 is shown. (D) Frequencies of IFN-γ+ NK cells in tumor are shown as Δ (PMA/Iono-unstimulated). (E) Numbers of tumor-infiltrating IFN-γ+ NK cells. (F) Δ MFI, [MFI-stimulated – MFI-unstimulated], of IFN-γ expression in tumor-infiltrating NK cells. Data are shown as mean ± SEM of 3 to 5 mice in each group and are representative of 3 independent experiments. Statistics: Student t test (A-B,D-F). lono, ionomycin; SSC, side scatter.
CD70 reverse signaling on NK cells is mediated via the AKT signaling pathway
To study the mechanism by which CD70 reverse signaling enhances NK cell activity, we stimulated NK cells with an anti-Ly49D mAb in the presence or absence of an activating anti-CD70 mAb (6D8).37 Co-stimulation of CD70 increased the frequency of IFN-γ+ CD107α+ activated NK cells after stimulation with anti-Ly49D mAb (Figure 4A-B). The increase of activated NK cells was mainly due to elevated numbers of IFN-γ–producing NK cells, whereas the frequency of CD107α+ NK cells remained unchanged or even slightly dropped (supplemental Figure 3A-B). In addition, the IFN-γ production per cell was increased by CD70 costimulation as indicated by a higher MFI of the IFN-γ staining (Figure 4C). The higher frequency of IFN-γ-producing NK cells upon anti-CD70 stimulation was further confirmed by coculturing irradiated MC57 or MC57-CD27-trunc cells with purified naive NK cells. Supernatants from MC57-CD27-trunc cocultures contained higher amounts of IFN-γ compared with MC57 cocultures (Figure 4D). Importantly, costimulation with anti-CD70 mAb (6D8) increased the frequency of Annexin-V− viability-dye− viable NK cells (Figure 4E-F). Increased viable cells frequency resulted in higher numbers of viable NK cells in anti-Ly49D-stimulated NK cells (supplemental Figure 3C). Therefore, CD70 reverse signaling enhanced the survival of NK cells.
Intracellular CD70 reverse signaling pathway. (A-C) FACS-sorted NK cells were stimulated for 4 hours with 0.5 μg/mL α-Ly49D or control rat IgG (rIgG, unstimulated) in the presence of Armenian Hamster IgG (IgG; 5 μg/mL) or activating anti-CD70 (6D8; 5 μg/mL). NK cells were stained intracellularly for IFN-γ and CD107α. (A) Representative FACS plots showing frequencies of NK cell subsets in anti-Ly49D–activated NK cells. (B) Frequency of IFN-γ+ CD107α+ NK cells. (C) Δ MFI [MFI-stimulated – MFI-unstimulated] of IFN-γ staining in NK cells. (D) FACS-sorted NK cells (105) were cocultured with irradiated 4 × 104 MC57 or MC57-CD27-trunc cells (35 Gy), in the presence of 40 U/mL interleukin-2. IFN-γ concentration in supernatants after 2 days is shown. NK cells alone supplemented with 50 ng/mL interleukin-18 were used as positive controls. (E-F) NK cells were stained with Annexin-V (AnxV) and viability dye (VD) after 16 hours of activation with anti-Ly49D and anti-CD70 or isotype control and analyzed by FACS. (E) Frequency of AnxV−VD− viable cells. (F) Representative FACS plot showing AnxV and VD staining out of 3 is shown. Data are shown as mean ± SEM of 3 wells and represent 3 independent experiments. (G-I) FACS-sorted NK cells were stimulated with 5 μg/mL anti-Ly49D antibody in the presence of 10 μg/mL anti-CD70 antibody (6D8) or control IgG for 0, 5, 15, 30, and 45 minutes. Phosphorylation of AKT and ERK was assessed by FACS. (G-H) MFI of p-AKT+ and p-ERK+ NK cells. (I) Representative FACS plots of p-AKT and p-ERK expression in NK cells 15 minutes after stimulation. Data are shown as mean ± SEM of triplicates and are representative of 3 different experiments. Statistics: Student t test (B-E), 2-way ANOVA (G-H). stim, stimulation.
Intracellular CD70 reverse signaling pathway. (A-C) FACS-sorted NK cells were stimulated for 4 hours with 0.5 μg/mL α-Ly49D or control rat IgG (rIgG, unstimulated) in the presence of Armenian Hamster IgG (IgG; 5 μg/mL) or activating anti-CD70 (6D8; 5 μg/mL). NK cells were stained intracellularly for IFN-γ and CD107α. (A) Representative FACS plots showing frequencies of NK cell subsets in anti-Ly49D–activated NK cells. (B) Frequency of IFN-γ+ CD107α+ NK cells. (C) Δ MFI [MFI-stimulated – MFI-unstimulated] of IFN-γ staining in NK cells. (D) FACS-sorted NK cells (105) were cocultured with irradiated 4 × 104 MC57 or MC57-CD27-trunc cells (35 Gy), in the presence of 40 U/mL interleukin-2. IFN-γ concentration in supernatants after 2 days is shown. NK cells alone supplemented with 50 ng/mL interleukin-18 were used as positive controls. (E-F) NK cells were stained with Annexin-V (AnxV) and viability dye (VD) after 16 hours of activation with anti-Ly49D and anti-CD70 or isotype control and analyzed by FACS. (E) Frequency of AnxV−VD− viable cells. (F) Representative FACS plot showing AnxV and VD staining out of 3 is shown. Data are shown as mean ± SEM of 3 wells and represent 3 independent experiments. (G-I) FACS-sorted NK cells were stimulated with 5 μg/mL anti-Ly49D antibody in the presence of 10 μg/mL anti-CD70 antibody (6D8) or control IgG for 0, 5, 15, 30, and 45 minutes. Phosphorylation of AKT and ERK was assessed by FACS. (G-H) MFI of p-AKT+ and p-ERK+ NK cells. (I) Representative FACS plots of p-AKT and p-ERK expression in NK cells 15 minutes after stimulation. Data are shown as mean ± SEM of triplicates and are representative of 3 different experiments. Statistics: Student t test (B-E), 2-way ANOVA (G-H). stim, stimulation.
CD70 reverse signaling in CD70-transgenic B cells has been shown to be mediated via the AKT and the extracellular signal-regulated kinase (ERK) signaling pathways.37,40 Stimulation with the anti-CD70 antibody (6D8) resulted in a higher frequency of phospho-AKT+ (p-AKT+) NK cells 15 minutes after activation (supplemental Figure 3D) as well as in an increased MFI of the p-AKT staining (Figure 4G,I). In contrast, CD70 reverse signaling did not change the expression of phospho-ERK (p-ERK) by NK cells (Figure 4H,I; supplemental Figure 3E). This data suggest that CD70 reverse signaling in NK cells increases effector function and cell survival via the AKT signaling pathway.
CD27-trunc expressed on lymphoma cells increases NK cell numbers and function
The MC57-CD27-trunc tumors allowed the study of the role of CD70 reverse signaling on NK cells in tumor control in a model that neither expresses CD27 nor CD70 in parental cells. However, CD27 is not expressed on solid tumors but on a majority of B-cell malignancies.10 Therefore, we studied the role of CD70 reverse signaling in Eµ-myc transgenic mice that develop aggressive B-cell lymphoma, resembling Burkitt lymphoma in humans. We established monoclonal cell lines from Eµ-myc lymphoma-bearing mice. A cell line that expressed neither CD27 nor CD70 on the cell surface (Q2A) was transduced with a Cd27-trunc GFP-expressing lentiviral construct (Q2A-CD27-trunc) or an empty vector (Q2A-empty) as a control (supplemental Figure 4A). The expression of MHC-I and NK cell ligands was comparable between Q2A-empty or Q2A-CD27-trunc cells (supplemental Figure 4B).
Twelve days after SC inoculation, Q2A-empty lymphomas grew to a bigger volume as Q2A-CD27-trunc lymphomas (Figure 5A). The absolute numbers and frequencies of lymphoma-infiltrating CD3− NK1.1+ NK cells were significantly higher in Q2A-CD27-trunc lymphomas than in controls (Figure 5B-C). This increase in NK cells was due to a better survival of NK cells in Q2A-CD27-trunc lymphomas, demonstrated by lower frequencies of Annexin-V+ apoptotic NK cells (Figure 5D). In addition, the expression of CD27-trunc on lymphoma cells increased the frequency of activated KLRG1+ lymphoma-infiltrating NK cells (Figure 5E). Moreover, the numbers and frequencies of IFN-γ+ NK were increased in CD27-trunc–expressing lymphoma after restimulation with PMA/ionomycin or anti-Ly49D antibody (Figure 5F; supplemental Figure 5A). Blocking CD70 by the mAb FR70 reduced the numbers of IFN-γ+ NK cells in Q2A-CD27-trunc to those in Q2A-empty lymphomas (Figure 5F; supplemental Figure 5A). Analyzing the MFI of IFN-γ staining revealed that activated NK cells in the Q2A-CD27-trunc lymphomas produced higher amounts of IFN-γ per cell than NK cells isolated from control lymphomas (Figure 5H-I). In line with the MC57 model, CD70 reverse signaling did not significantly increase the number of CD107α-expressing NK cells (Figure 5G; supplemental Figure 5A). Our data indicate that CD27-trunc expression on lymphoma cells increases the number and function of lymphoma-infiltrating NK cells.
CD27-trunc expression on lymphoma cells increases NK cell numbers and function. (A) Volume of Q2A-CD27-trunc and Q2A-empty lymphomas after 12 days SC injection into BL/6 mice. (B) Representative FACS plot showing frequency of NK cells in lymphoma-infiltrating leukocytes. (C) Numbers of lymphoma-infiltrating NK cells. (D) Frequency of Annexin-V+ NK cells. (E) Frequency of KLRG1+ NK cells. (F-G) Cell suspensions from tumors at day 12 were restimulated with PMA/ionomycin or anti-Ly49D–activating mAb, in the presence of anti-CD70 blocking antibody (FR70) or control IgG, and IFN-γ and CD107α expression was analyzed on CD19− CD3− NK1.1+ NK cells by FACS. (F) Numbers of IFN-γ+ NK cells. (G) Numbers of CD107α+ NK cells. (H) Histogram showing the expression of IFN-γ in lymphoma-infiltrating NK cells after PMA/ionomycin restimulation, for 3 tumor samples in each condition. (I) Δ MFI, [MFI-stimulated – MFI-unstimulated], of IFN-γ in Q2A-empty and Q2A-CD27-trunc lymphoma-infiltrating NK cells. Data are shown as mean ± SEM of 3 animals in each group (A-I) and are representative of 3 independent experiments. Statistics: Student t test (A,C-G,I).
CD27-trunc expression on lymphoma cells increases NK cell numbers and function. (A) Volume of Q2A-CD27-trunc and Q2A-empty lymphomas after 12 days SC injection into BL/6 mice. (B) Representative FACS plot showing frequency of NK cells in lymphoma-infiltrating leukocytes. (C) Numbers of lymphoma-infiltrating NK cells. (D) Frequency of Annexin-V+ NK cells. (E) Frequency of KLRG1+ NK cells. (F-G) Cell suspensions from tumors at day 12 were restimulated with PMA/ionomycin or anti-Ly49D–activating mAb, in the presence of anti-CD70 blocking antibody (FR70) or control IgG, and IFN-γ and CD107α expression was analyzed on CD19− CD3− NK1.1+ NK cells by FACS. (F) Numbers of IFN-γ+ NK cells. (G) Numbers of CD107α+ NK cells. (H) Histogram showing the expression of IFN-γ in lymphoma-infiltrating NK cells after PMA/ionomycin restimulation, for 3 tumor samples in each condition. (I) Δ MFI, [MFI-stimulated – MFI-unstimulated], of IFN-γ in Q2A-empty and Q2A-CD27-trunc lymphoma-infiltrating NK cells. Data are shown as mean ± SEM of 3 animals in each group (A-I) and are representative of 3 independent experiments. Statistics: Student t test (A,C-G,I).
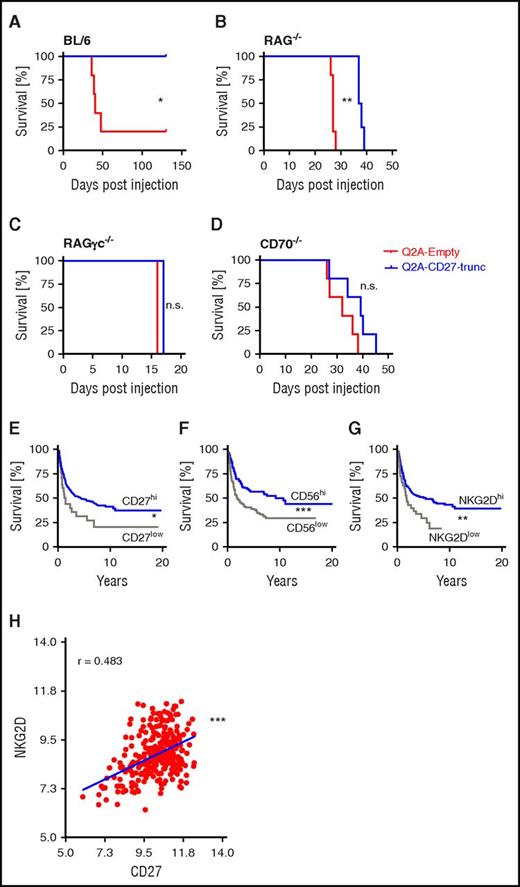
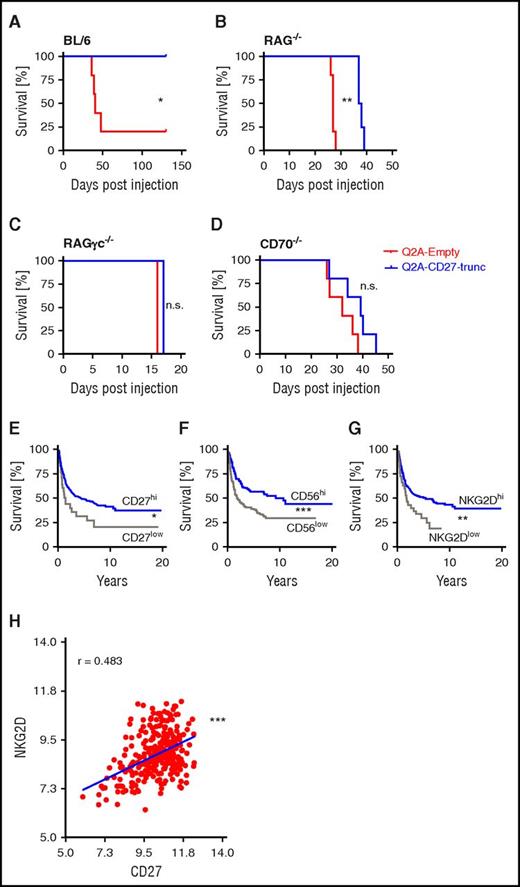
CD70 reverse signaling prolongs survival in high-grade lymphomas
To analyze a lymphoma that develops more physiologically in different lymph nodes in the body, we injected Q2A-CD27-trunc or Q2A-empty lymphoma cells IV into recipient mice. BL/6 mice injected with Q2A-CD27-trunc lymphomas did not develop detectable lymphomas and survived long term. In contrast, most control mice injected with Q2A-empty lymphoma cells died within 50 days (Figure 6A). Similarly, survival of RAG−/− mice injected with Q2A-CD27-trunc lymphoma was significantly longer than after injection with control Q2A-empty lymphoma cells (Figure 6B). In contrast, survival was identical when Q2A-CD27-trunc and Q2A-empty lymphoma cells were injected into RAGγc−/− or CD70−/− mice (Figure 6C-D). These experiments indicate that CD70 reverse signaling induced by CD27-trunc expressing lymphoma cells activates NK cells.
CD27 expression on lymphoma cells prolongs survival. (A-D) Kaplan-Meier survival curves of BL/6 (A), RAG−/− (B), RAGγc−/− (C), and CD70−/− (D) mice, injected IV with Q2A-CD27-trunc or Q2A-empty lymphoma cells. (E-G) Kaplan-Meier survival curve of 303 patients with Burkitt lymphoma and DLBCL in correlation with the expression of CD27 (CD27hi n = 268, CD27low n = 35) (E), CD56 (CD56hi n = 201, CD56low n = 102) (F), and NKG2D (NKG2Dhi n = 272, NKG2Dlow = 31) (G). (H) Correlation analysis of expression of NK cell marker NKG2D and CD27 in lymphoma patients. Data are shown as mean ± SEM of 4 to 5 animals in each group (A-D) and representative of 2 experiments. Statistics: log-rank analysis (A-G). Spearman correlation test (H).
CD27 expression on lymphoma cells prolongs survival. (A-D) Kaplan-Meier survival curves of BL/6 (A), RAG−/− (B), RAGγc−/− (C), and CD70−/− (D) mice, injected IV with Q2A-CD27-trunc or Q2A-empty lymphoma cells. (E-G) Kaplan-Meier survival curve of 303 patients with Burkitt lymphoma and DLBCL in correlation with the expression of CD27 (CD27hi n = 268, CD27low n = 35) (E), CD56 (CD56hi n = 201, CD56low n = 102) (F), and NKG2D (NKG2Dhi n = 272, NKG2Dlow = 31) (G). (H) Correlation analysis of expression of NK cell marker NKG2D and CD27 in lymphoma patients. Data are shown as mean ± SEM of 4 to 5 animals in each group (A-D) and representative of 2 experiments. Statistics: log-rank analysis (A-G). Spearman correlation test (H).
To determine whether the expression of CD27 correlates with improved survival in aggressive lymphoma in humans, we took advantage of a published gene expression array dataset from 303 patients with aggressive lymphomas (71 Burkitt lymphomas and 232 DLBCLs).48 To assess CD27 messenger RNA (mRNA) expression in relation to overall survival, we performed a cut-point selection for the CD27 expression using the “X-tile” method (supplemental material).49 An optimal cut point of 8.74 was determined to define CD27low- and CD27high-expressing patients. Using this threshold for the entire cohort, Kaplan-Meier analysis revealed that patients with high CD27 mRNA expression (>8.74) survived significantly longer than patients with low CD27 mRNA expression (≤8.74) (Figure 6E).
In addition, the expression of CD56 and NKG2D, as an indicator for NK cell infiltration in the lymphoma, was analyzed in relation to overall survival. Similarly, optimal thresholds were determined as 4.49 and 7.36 for CD56 and NKG2D, respectively. Survival was better for patients with high expression of the NK cell markers CD56 and NKG2D than patients with low infiltration of NK cells (Figure 6F-G). Importantly, the expression of the NK cell marker NKG2D correlated with the expression of CD27 in the lymphoma samples (Figure 6H). As shown before,50,51 tumor- or lymphoma-infiltrating T cells correlated with a better prognosis (supplemental Figure 6A-B). However, there was no or only a very weak correlation between the expression of T-cell markers CD4 and CD8 and CD27 (supplemental Figure 6C-D). This exploratory correlative analysis fits with the hypothesis that CD70-reverse signaling increases NK cell function in vivo.
CD70 reverse signaling enhances NK cell survival and function in ALL xenotransplants
In order to study CD70 reverse signaling in human NK cells, we coincubated allogeneic human NK cells (FACS-sorted for CD27 negativity) with the human lymphoma cell line Oci-Ly1 and with primary human B-ALL cells (FACS-sorted for CD70 negativity) (supplemental Figure 7A-B). Blocking CD70 signaling by anti-CD70 mAb (41D12D)52,53 resulted in decreased frequencies of IFN-γ+ CD107α+ double-positive NK cells (Figure 7A). CD70 blocking slightly increased the frequency of Annexin V+ NK cells (Figure 7B). In contrast, the frequency of Annexin V+ B cells did not change upon CD70 blocking, indicating that CD27 forward signaling did not trigger antiapoptotic mechanisms in our model (supplemental Figure 7C). Despite the decrease of CD107α+ NK cells upon CD70 blocking, the lysis of the Oci-Ly1 and K562 cells was independent of CD70 reverse signaling (supplemental Figure 7D-E). Blocking important effector molecules of NK cells revealed that cytotoxicity against Oci-Ly1 cells was mediated by granzyme B but not the interaction of Fas ligand (FasL) and Fas receptor (Fas) (supplemental Figure 7F).
CD70 reverse signaling in human NK cells. (A-B) CD70-negative- CD27-positive- Oci-Ly1 or primary B-ALL cells (patient 1, supplemental Table 1) were cocultured with FACS-sorted CD27-negative NK cells from healthy donors at a ratio of 5:1, in the presence of blocking anti-CD70 antibody or IgG. After 48 hours, IFN-γ and CD107α expression was analyzed. (A) Frequency of IFN-γ+ CD107α+ NK cells. (B) Frequency of Annexin-V+ NK cells. (C-J) Human B-ALL cells (5 × 106; patient 2; supplemental Table 1) were injected IV into NSG mice and analyzed for engraftment in blood at the time points indicated. B-ALL–bearing mice with 5% to 10% engraftment were injected IV with FACS-sorted human NK cells (5 × 106) and treated with anti-CD70 or IgG for 48 hours. (D) Human CD56+ CD3− NK cell numbers in spleens of B-ALL–bearing mice 2 days after NK cell transfer. (E-I) Restimulation of CD19-MACS–depleted splenocytes with PMA/ionomycin. (E-F) Frequencies of IFN-γ+ (E) and IFN-γ+ CD107α+ (F) human NK cells. (G) Δ MFI, [MFI-stimulated – MFI-unstimulated], of IFN-γ in NK cells. (H) Frequency of CD107α+ NK cells. (I) Frequency of Annexin-V+ NK cells. (J) MFI of CD70 on NK cells. Data are shown as mean ± SEM of triplicates per group in panels A-B and 3 animals per group in panels C-J representative of 3 independent experiments. Statistics: Student t test (A-B,D-J). hNK, human NK; PB, peripheral blood.
CD70 reverse signaling in human NK cells. (A-B) CD70-negative- CD27-positive- Oci-Ly1 or primary B-ALL cells (patient 1, supplemental Table 1) were cocultured with FACS-sorted CD27-negative NK cells from healthy donors at a ratio of 5:1, in the presence of blocking anti-CD70 antibody or IgG. After 48 hours, IFN-γ and CD107α expression was analyzed. (A) Frequency of IFN-γ+ CD107α+ NK cells. (B) Frequency of Annexin-V+ NK cells. (C-J) Human B-ALL cells (5 × 106; patient 2; supplemental Table 1) were injected IV into NSG mice and analyzed for engraftment in blood at the time points indicated. B-ALL–bearing mice with 5% to 10% engraftment were injected IV with FACS-sorted human NK cells (5 × 106) and treated with anti-CD70 or IgG for 48 hours. (D) Human CD56+ CD3− NK cell numbers in spleens of B-ALL–bearing mice 2 days after NK cell transfer. (E-I) Restimulation of CD19-MACS–depleted splenocytes with PMA/ionomycin. (E-F) Frequencies of IFN-γ+ (E) and IFN-γ+ CD107α+ (F) human NK cells. (G) Δ MFI, [MFI-stimulated – MFI-unstimulated], of IFN-γ in NK cells. (H) Frequency of CD107α+ NK cells. (I) Frequency of Annexin-V+ NK cells. (J) MFI of CD70 on NK cells. Data are shown as mean ± SEM of triplicates per group in panels A-B and 3 animals per group in panels C-J representative of 3 independent experiments. Statistics: Student t test (A-B,D-J). hNK, human NK; PB, peripheral blood.
To study CD70 reverse signaling in human NK cells in vivo, we established a human B-ALL xenograft in immunocompromised NSG mice. The transplanted B-ALL cells expressed CD27 but not CD70 (supplemental Figure 7B). Recipient mice were monitored by repetitive bleedings until they had 5% to 10% of ALL engraftment (Figure 7C). Then, FACS-sorted CD27-negative allogenic human NK cells were adoptively transferred into ALL-bearing recipients. Mice were randomized to either treatment with blocking anti-CD70 Ab52,53 or isotype control (Figure 7C). Blocking the CD27/CD70 interaction significantly reduced the number of total human NK cells (Figure 7D) as well as the frequency of IFN-γ+ and IFN-γ+CD107α+ human NK cells in spleen (Figure 7E-F; supplemental Figure 7G). In addition, treatment with anti-CD70 mAb reduced the IFN-γ production per NK cell (Figure 7G). Similarly to the experiments with syngenic tumors, CD70 reverse signaling did not increase the frequency of CD107α+ NK cells (Figure 7H). The CD70/CD27 interaction increased survival of the transferred NK cells as indicated by lower frequencies of Annexin V+ cells (Figure 7I). However, the frequency of apoptotic malignant B cells remained unchanged in anti-CD70 Ab or immunoglobulin G (IgG)-treated mice. The comparable survival of malignant B cells is probably due to the low effector:target ratio (1:1000, ∼3 × 104 NK cells: ∼4 × 107 B cells in spleen) and to the short timespan of interaction with malignant cells. Importantly, CD70 expression on NK cells was only detectable in anti-CD70–treated but not in control animals, indicating ligation in vivo (Figure 7J; supplemental Figure 7H47 ). Similarly, CD70 was highly expressed on mRNA level in NK cells in peripheral blood of B-ALL patients at diagnosis, but CD70 surface expression as analyzed by FACS was low, suggesting CD70 engagement in vivo in patients (supplemental Figure 8A,C,D). Together, these studies with allogenic NK cells in human B-ALL xenografts confirm that CD27 expressed on malignant B cells induces activation and survival of CD70-expressing NK cells.
Discussion
One major reason for NHL development is the escape of transformed B cells from the constant immunosurveillance by immune cells. The incidence of Epstein-Barr virus (EBV)-associated aggressive NHL is substantially increased in immunodeficient patients.54,55 EBV-derived antigen LMP1 expressed in B cells is a strong lymphoma-associated antigen that activates specific cytotoxic T cells. Recently, Afshar-Sterle et al demonstrated that T cells prevent spontaneous lymphoma development caused by mutations that block an intrinsic cellular differentiation pathway by FAS ligand-mediated cytotoxicity.56 However, other effector functions such as killing through perforin and granzyme and cytokine-mediated cytotoxicity may contribute to the immune control of lymphoma cells.57,58 B-cell lymphomas frequently exhibit a downregulation of immunogenic molecules, such as MHC and costimulatory molecules that render them unrecognizable for effector T cells.59-61 Altered immunogenicity of malignant B cells strongly indicates that lymphoma cells are under a selective pressure to escape the immunosurveillance by the adaptive immunity. Unlike T cells, NK cells do not need tumor antigen presentation to be activated; however, they integrate danger signals that they receive through their activating and inhibitory receptors.62,63
Although the role of cytotoxic T and NK cells in the immunosurveillance of lymphoma is well documented, the molecular mechanisms regulating the immune control are poorly understood. We here analyzed the role of CD27 expression on malignant B cells in the immunosurveillance of B-cell malignancies. CD27 usually acts as a receptor, and intracellular signaling leads to antiapoptotic and proliferative signals. It is therefore conceivable that similar to normal lymphocytes, CD27 signaling on malignant B cells leads to lymphoma progression.8,14 However, many members of the TNFR ligand family, such as CD40L, LIGHT, and also CD70, have been reported to have reverse signaling activity and are involved in the activation of lymphocytes.25,37,40 Aberrant expression of CD70 and CD27 on both lymphoma and lymphoma-infiltrating immune cells leads to simultaneous signaling downstream of both cellular receptors. Therefore, in order to study CD70 reverse signaling in immune cells, independently from the forward signaling of CD27 in lymphoma cells, we established an experimental tumor model in which CD27 signaling is blocked, yet a cellular ligand for CD70 on immune cells is provided. Blocking CD27 signaling was fulfilled by expressing a cytoplasmic deletion mutant of CD27 receptor (CD27-truncated) on FACS-sorted CD27- and CD70-double-negative lymphoma cells from Eµ-myc transgenic mice. However, in this experimental setting, we cannot exclude upregulation of CD27 or CD70 in vivo. Therefore, a fibrosarcoma cell line, which lacks both CD27 and CD70, was used to unambiguously assess CD70 reverse signaling. Our results revealed that CD70 reverse signaling increased the numbers of tumor- or lymphoma-infiltrating activated NK cells leading to improved tumor control. Analysis of tumor-infiltrating NK cells revealed that CD70 reverse signaling reduced apoptosis and increased effector function, as analyzed by IFN-γ production after in vitro restimulation. In the Burkitt lymphoma–like model, the improved NK cell–mediated immune control significantly prolonged survival. Similarly, CD70 reverse signaling induced IFN-γ production and reduced apoptosis of human NK cells in vitro. In agreement with our experimental data, an explorative analysis of an mRNA expression array of DLBCL and Burkitt lymphoma from patients confirmed a better prognosis for patients with CD27high-expressing lymphomas. Although we cannot distinguish between CD27 expressed on lymphoma-infiltrating immune cells and malignant B cells, the majority of the analyzed cells in the array represent malignant cells. Moreover, sCD27 as an indicator of CD27 ligation clearly correlates with lymphoma load.8 Importantly, the level of CD27 expression in the lymphoma samples correlated with NK cell infiltration, as analyzed by the expression of the NK cell marker NKG2D. In addition, we documented an important role of CD70 reverse signaling in the activation of and survival of NK cells in a human B-ALL xenograft model. Consistent with our hypothesis, patients lacking functional CD27 or CD70 are at risk to develop aggressive B-cell lymphoma.64,65 However, because the CD27/CD70 interaction is crucially involved in the immune control of EBV,66 these studies do not allow the determination of a direct role of the CD27/CD70 signaling on the immune control of the lymphoma.
In vitro activation by agonistic CD70 mAbs in combination with the NK stimulating antibody anti-Ly49D suggested that intracellular CD70 reverse signaling is mainly mediated via the AKT pathway. Similarly, the AKT pathway is involved in CD70 reverse signaling in CD70 transgenic B cells in vivo, whereas in contrast to this model, we could not document a role of the ERK signaling pathway.37 This discrepancy may be due to the different lymphocyte subset studied or to higher expression levels of CD70 in the transgenic model. Our results are in agreement with earlier in vitro experiments documenting that CD70 can act as a signal-transducing molecule in activated CD70+ NK cells.40 Our in vivo experiments suggested that CD70 reverse signaling led to NK cell activation and survival but did not enhance the activity of cytotoxic T cells. This result was surprising because both MC57 fibrosarcoma and Q2A lymphoma cells expressed MHC-class I, and CD70 reverse signaling has also been documented in T-cell clones and Jurkat cells in vitro.39 However, our results suggest that tumor-infiltrating effector T cells are less dependent on CD70 reverse signaling. Our hypothesis is in line with a recent report indicating that CD27 rather than CD70 on T lymphocytes is crucial for T-cell activity against EBV-induced lymphomas.66
The CD70/CD27 signaling axis is a promising target for cancer immunotherapy. CD70-transfected dendritic cells and agonistic CD27-specific antibodies are currently tested in preclinical and clinical trials.67,68 In addition, due to the very limited expression on activated lymphocytes and on some tumor cells, strategies to target CD70-expressing cells with immunoconjugates or antibodies with enhanced antibody-dependent cellular cytotoxicity are exploited.31,52 We recently documented that CD27 signaling increases the frequency of regulatory T cells in solid tumors and promoted tumor growth.43 Therefore, blocking CD27 signaling led to rejection of tumors that are mainly controlled by cytotoxic T cells. In addition, in chronic myelogenous leukemia, CD27 signaling increased the expansion of leukemia stem cells and led to disease progression.69 Our current study now indicates that CD70 reverse signaling in NK cells increases the immune control of CD27-expressing lymphoma cells. Bidirectional activity of the CD27/CD70 axis indicates that strategies that therapeutically target the CD70/CD27 axis in cancer immunotherapy are different depending on the cancer type and the preexisting antitumoral immune response.
The online version of this article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
The authors thank Martijn Nolte for providing the anti-CD70 mAb (6D8); Jonathan Ashwell for providing the Cd70−/− mice and critical reading of the paper; and Jean-Pierre Bourquin and Beat C. Bornhauser for providing the ALL xenotransplants.
This work was supported by the Swiss National Science Foundation (31003A_149768, 310030B_133132, 310030-156407), the Swiss Cancer League (KFS-2879-02-2012), the Cancer League of the Canton of Bern, the Werner und Hedy Berger-Janser-Stiftung, the Bernese Foundation for Clinical Cancer Research, the Marlies Schwegler-Stiftung, and the Stiftung Kinderkrebsforschung Schweiz.
Authorship
Contribution: M.F.A.S. designed and performed the experiments, interpreted the data, prepared the figures, and wrote the paper; C.A.R., T.H., C.C., and R.R. performed experiments; J.-P.B. and B.C.B. contributed to the establishment of B-ALL xenograft model and provided B-ALL cells; C.R. prepared figures, designed experiments, and wrote the paper; and A.F.O. designed and supervised experiments and wrote the paper.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
The current affiliation for C.C. is Tumor Immunology, Roche Pharmaceutical Research and Early Development, Roche Innovation Center Zurich, Schlieren, Switzerland.
Correspondence: Adrian F. Ochsenbein, Department of Medical Oncology, Inselspital, University Hospital and University of Bern, 3010 Bern, Switzerland; e-mail: adrian.ochsenbein@insel.ch.

![Figure 3. CD27-trunc enhances the activity of tumor-infiltrating NK cells. (A-F) Analysis of NK cells in spleens (A) and tumor tissue (B-F) of MC57 or MC57-CD27-trunc tumor-bearing mice, 12 days after tumor transplantation. (A) Frequencies and numbers of NK cells in spleens of BL/6 mice. (B) Numbers of tumor-infiltrating NK cells. (C-F) MACS-sorted CD45+ cells from tumor tissue were restimulated with PMA/ionomycin for 4 hours and IFN-γ was analyzed by FACS. (C) One representative FACS plot of IFN-γ+ NK cells out of 3 is shown. (D) Frequencies of IFN-γ+ NK cells in tumor are shown as Δ (PMA/Iono-unstimulated). (E) Numbers of tumor-infiltrating IFN-γ+ NK cells. (F) Δ MFI, [MFI-stimulated – MFI-unstimulated], of IFN-γ expression in tumor-infiltrating NK cells. Data are shown as mean ± SEM of 3 to 5 mice in each group and are representative of 3 independent experiments. Statistics: Student t test (A-B,D-F). lono, ionomycin; SSC, side scatter.](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/130/3/10.1182_blood-2016-12-756585/4/m_blood756585f3.jpeg?Expires=1765005749&Signature=AVoe15zrJ-6bzW4aKiHFWZvBQvcAN-lL8GfBTwO-5TvIJGVvzCezhca1Q6yhQMbZY5eiU5C0Hew7f5iTwWHedppkc8NixPEt57rM4Gnnh4KAwgAd4mzYYjpU2OYjcmLIb~SubBq41pyoYKGoSVmlUI~usyg-M~vNZCrXPUQoGPtADgo2-8~oktiVSsbNppI-WXrc1TqzLF5Q5~cVJ6a8Gj5X~3VbOnX-p2TKVrWtM-JaCym6LehxU~ORKwrB2ri7is0dBeEvl7GJ~MKvbUdpbrLpLCaW1p5Kd77sJP3x3L3J1jesmLR02G-L7bhYn5RWJKei9ft8NBryPKe9lxjCtw__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)
![Figure 4. Intracellular CD70 reverse signaling pathway. (A-C) FACS-sorted NK cells were stimulated for 4 hours with 0.5 μg/mL α-Ly49D or control rat IgG (rIgG, unstimulated) in the presence of Armenian Hamster IgG (IgG; 5 μg/mL) or activating anti-CD70 (6D8; 5 μg/mL). NK cells were stained intracellularly for IFN-γ and CD107α. (A) Representative FACS plots showing frequencies of NK cell subsets in anti-Ly49D–activated NK cells. (B) Frequency of IFN-γ+ CD107α+ NK cells. (C) Δ MFI [MFI-stimulated – MFI-unstimulated] of IFN-γ staining in NK cells. (D) FACS-sorted NK cells (105) were cocultured with irradiated 4 × 104 MC57 or MC57-CD27-trunc cells (35 Gy), in the presence of 40 U/mL interleukin-2. IFN-γ concentration in supernatants after 2 days is shown. NK cells alone supplemented with 50 ng/mL interleukin-18 were used as positive controls. (E-F) NK cells were stained with Annexin-V (AnxV) and viability dye (VD) after 16 hours of activation with anti-Ly49D and anti-CD70 or isotype control and analyzed by FACS. (E) Frequency of AnxV−VD− viable cells. (F) Representative FACS plot showing AnxV and VD staining out of 3 is shown. Data are shown as mean ± SEM of 3 wells and represent 3 independent experiments. (G-I) FACS-sorted NK cells were stimulated with 5 μg/mL anti-Ly49D antibody in the presence of 10 μg/mL anti-CD70 antibody (6D8) or control IgG for 0, 5, 15, 30, and 45 minutes. Phosphorylation of AKT and ERK was assessed by FACS. (G-H) MFI of p-AKT+ and p-ERK+ NK cells. (I) Representative FACS plots of p-AKT and p-ERK expression in NK cells 15 minutes after stimulation. Data are shown as mean ± SEM of triplicates and are representative of 3 different experiments. Statistics: Student t test (B-E), 2-way ANOVA (G-H). stim, stimulation.](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/130/3/10.1182_blood-2016-12-756585/4/m_blood756585f4.jpeg?Expires=1765005749&Signature=zyiKYrIJPXdBV1L-qJjUuxc7590oZXyCASC6m9g0e77eOobIFTiLLfMyb0kP5KagakUE3TlAHrPINNDZan1xQQwo6qX08F1RDWKKnBPmWsb0-A4cT5-~8KEAnxX4eH0y6QI~FH0CubiawZDKO8ZADBCUHmwZfOBxBtEVMh6N5z3nchy9nrG0R53dpK5LFzAYetPBwpFmF-k8QmEVzbENtZOzYlcTpGrNk9P~xHtGXJoEZyrVpwkKgnaaH1VlHRFzNImiaQr~9YkJwDu5MUwsdo7ymvqoZC4ldD20yv4QDHnjbw7CzbUHMEIWBA28Th-d5jwXhuq-lIsr10L0i1kWTA__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)
![Figure 5. CD27-trunc expression on lymphoma cells increases NK cell numbers and function. (A) Volume of Q2A-CD27-trunc and Q2A-empty lymphomas after 12 days SC injection into BL/6 mice. (B) Representative FACS plot showing frequency of NK cells in lymphoma-infiltrating leukocytes. (C) Numbers of lymphoma-infiltrating NK cells. (D) Frequency of Annexin-V+ NK cells. (E) Frequency of KLRG1+ NK cells. (F-G) Cell suspensions from tumors at day 12 were restimulated with PMA/ionomycin or anti-Ly49D–activating mAb, in the presence of anti-CD70 blocking antibody (FR70) or control IgG, and IFN-γ and CD107α expression was analyzed on CD19− CD3− NK1.1+ NK cells by FACS. (F) Numbers of IFN-γ+ NK cells. (G) Numbers of CD107α+ NK cells. (H) Histogram showing the expression of IFN-γ in lymphoma-infiltrating NK cells after PMA/ionomycin restimulation, for 3 tumor samples in each condition. (I) Δ MFI, [MFI-stimulated – MFI-unstimulated], of IFN-γ in Q2A-empty and Q2A-CD27-trunc lymphoma-infiltrating NK cells. Data are shown as mean ± SEM of 3 animals in each group (A-I) and are representative of 3 independent experiments. Statistics: Student t test (A,C-G,I).](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/130/3/10.1182_blood-2016-12-756585/4/m_blood756585f5.jpeg?Expires=1765005749&Signature=ptIQOdaJarZbST1HQ7GYUd3IDVgK6rvmAS4~Z~sJ8ro7GtvlmHCCqE0PIbWoM9L5lDvHp0HWZBMQ8aMVAtDfqCmgztE8j1BzXG3VfinVUwjvh0CofeTZF-B1zjHx1gr7S~M24la~CYyzQOrGQrJNTNTkio6up4QevMfBGj7q55lI1ujbEhA--mlAuQ~NLyRTLPr957gsQ6ZjSBoITzsWM8k5mMTQOIuWD1m4FBrAyW4M~bn5SUbvTXOXOIVNNh71WojOOXdGZZpbs3-v0LCzkr5Tb7~a70RPV7Ve66Kq0yX9go7AcvP9mhG1UGg6BmgPeCXOEFicFuseCxm0gx7QHw__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)
![Figure 7. CD70 reverse signaling in human NK cells. (A-B) CD70-negative- CD27-positive- Oci-Ly1 or primary B-ALL cells (patient 1, supplemental Table 1) were cocultured with FACS-sorted CD27-negative NK cells from healthy donors at a ratio of 5:1, in the presence of blocking anti-CD70 antibody or IgG. After 48 hours, IFN-γ and CD107α expression was analyzed. (A) Frequency of IFN-γ+ CD107α+ NK cells. (B) Frequency of Annexin-V+ NK cells. (C-J) Human B-ALL cells (5 × 106; patient 2; supplemental Table 1) were injected IV into NSG mice and analyzed for engraftment in blood at the time points indicated. B-ALL–bearing mice with 5% to 10% engraftment were injected IV with FACS-sorted human NK cells (5 × 106) and treated with anti-CD70 or IgG for 48 hours. (D) Human CD56+ CD3− NK cell numbers in spleens of B-ALL–bearing mice 2 days after NK cell transfer. (E-I) Restimulation of CD19-MACS–depleted splenocytes with PMA/ionomycin. (E-F) Frequencies of IFN-γ+ (E) and IFN-γ+ CD107α+ (F) human NK cells. (G) Δ MFI, [MFI-stimulated – MFI-unstimulated], of IFN-γ in NK cells. (H) Frequency of CD107α+ NK cells. (I) Frequency of Annexin-V+ NK cells. (J) MFI of CD70 on NK cells. Data are shown as mean ± SEM of triplicates per group in panels A-B and 3 animals per group in panels C-J representative of 3 independent experiments. Statistics: Student t test (A-B,D-J). hNK, human NK; PB, peripheral blood.](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/130/3/10.1182_blood-2016-12-756585/4/m_blood756585f7.jpeg?Expires=1765005749&Signature=SIeiPFODssqgJ0lGSwQptDq8VNjRDjJzH0SXgrE1hBUAgkFfaDKGlLMnj4vihMepOhsXnZqlSzk-gY6iQaiSmg-9cA5cN9OAX3cWkO4Ob-17KzkBc8EYsa7mNoC7qXIzwhmCkXd5rOq17nFmMROCrxR0S4-lxnSrDDyhSGf7WexbADji-abu6LNpmSjK3aIszcFrvyWM81gPjPPiMy8reM-7pzo8IXOyI4xh7JEiokg-S2-SGfTzSJyJ3CheymmtnqtG0JXrnwy5kJY1qXW4ozBWnd8ZD9Eqde~5om35AWDqa-wQ~PNycx0hZKX8KH1bdObxbSyPsjnqkZbevcZSoQ__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)

![Figure 3. CD27-trunc enhances the activity of tumor-infiltrating NK cells. (A-F) Analysis of NK cells in spleens (A) and tumor tissue (B-F) of MC57 or MC57-CD27-trunc tumor-bearing mice, 12 days after tumor transplantation. (A) Frequencies and numbers of NK cells in spleens of BL/6 mice. (B) Numbers of tumor-infiltrating NK cells. (C-F) MACS-sorted CD45+ cells from tumor tissue were restimulated with PMA/ionomycin for 4 hours and IFN-γ was analyzed by FACS. (C) One representative FACS plot of IFN-γ+ NK cells out of 3 is shown. (D) Frequencies of IFN-γ+ NK cells in tumor are shown as Δ (PMA/Iono-unstimulated). (E) Numbers of tumor-infiltrating IFN-γ+ NK cells. (F) Δ MFI, [MFI-stimulated – MFI-unstimulated], of IFN-γ expression in tumor-infiltrating NK cells. Data are shown as mean ± SEM of 3 to 5 mice in each group and are representative of 3 independent experiments. Statistics: Student t test (A-B,D-F). lono, ionomycin; SSC, side scatter.](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/130/3/10.1182_blood-2016-12-756585/4/m_blood756585f3.jpeg?Expires=1765507166&Signature=XZliu7WTlo9vKNGCQCYaTO3YRYyHZP0mU4v~lr3-kMttjJzRFOuOU8nVK~eRx324-be2W2-xBU-C8i4DR8HV1KZ58dNvx5RHWOmfvfirR95kBW93lH2msTt5GpFwi~-RffEBvFo-BkiIwhnCdB3JBnKPyHAWaIaNX-LMSrqzoZpYHKArB30phWe710U9B~2pfwrt~ipt9hbiiYbF-V5DmkWEzmrB0iAyp2z1FkhXQEFjtMDPKL90-4AKtorrw4Xmm1VflC47qcO7ZZJxIEps6DoQbXwJMA2AsJ~zJxH5TmDbQrGoe1sLVdZW7~lV~1nTVeMmUhPIZ-0YTNl4uZEbNA__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)
![Figure 4. Intracellular CD70 reverse signaling pathway. (A-C) FACS-sorted NK cells were stimulated for 4 hours with 0.5 μg/mL α-Ly49D or control rat IgG (rIgG, unstimulated) in the presence of Armenian Hamster IgG (IgG; 5 μg/mL) or activating anti-CD70 (6D8; 5 μg/mL). NK cells were stained intracellularly for IFN-γ and CD107α. (A) Representative FACS plots showing frequencies of NK cell subsets in anti-Ly49D–activated NK cells. (B) Frequency of IFN-γ+ CD107α+ NK cells. (C) Δ MFI [MFI-stimulated – MFI-unstimulated] of IFN-γ staining in NK cells. (D) FACS-sorted NK cells (105) were cocultured with irradiated 4 × 104 MC57 or MC57-CD27-trunc cells (35 Gy), in the presence of 40 U/mL interleukin-2. IFN-γ concentration in supernatants after 2 days is shown. NK cells alone supplemented with 50 ng/mL interleukin-18 were used as positive controls. (E-F) NK cells were stained with Annexin-V (AnxV) and viability dye (VD) after 16 hours of activation with anti-Ly49D and anti-CD70 or isotype control and analyzed by FACS. (E) Frequency of AnxV−VD− viable cells. (F) Representative FACS plot showing AnxV and VD staining out of 3 is shown. Data are shown as mean ± SEM of 3 wells and represent 3 independent experiments. (G-I) FACS-sorted NK cells were stimulated with 5 μg/mL anti-Ly49D antibody in the presence of 10 μg/mL anti-CD70 antibody (6D8) or control IgG for 0, 5, 15, 30, and 45 minutes. Phosphorylation of AKT and ERK was assessed by FACS. (G-H) MFI of p-AKT+ and p-ERK+ NK cells. (I) Representative FACS plots of p-AKT and p-ERK expression in NK cells 15 minutes after stimulation. Data are shown as mean ± SEM of triplicates and are representative of 3 different experiments. Statistics: Student t test (B-E), 2-way ANOVA (G-H). stim, stimulation.](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/130/3/10.1182_blood-2016-12-756585/4/m_blood756585f4.jpeg?Expires=1765507166&Signature=Ky-d4DPHqNUa9YGTRSE2spJgnY6xHKLE562FD0Au4EvDKhFJr-dEUC5OQTtXVGkQLje-yl49o4hxyIAa68utIs03Y-3yI7B7HIRdvuWxJBBs0f6snIrR-ls~ayYxMZM4CPcS50wjMYYtOcPBg4JQGK1YS0gqJok4fixqU6nMW7khoW9JHl3gLItaF9li0S2D0lZdM4v1NuWrC-5p596-8qPFF0WV7sfXjyr2o2HS4S5HjmdCM2vVZmjLgTjK8hFekWWbOqvhGdLmLf8jqyC6Pw4Weu-SG4gWmhcHgEfrMMRIJhWzIMIcjttxMbwo-QYF0TBs5oOsKwbour2vdDfK~g__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)
![Figure 5. CD27-trunc expression on lymphoma cells increases NK cell numbers and function. (A) Volume of Q2A-CD27-trunc and Q2A-empty lymphomas after 12 days SC injection into BL/6 mice. (B) Representative FACS plot showing frequency of NK cells in lymphoma-infiltrating leukocytes. (C) Numbers of lymphoma-infiltrating NK cells. (D) Frequency of Annexin-V+ NK cells. (E) Frequency of KLRG1+ NK cells. (F-G) Cell suspensions from tumors at day 12 were restimulated with PMA/ionomycin or anti-Ly49D–activating mAb, in the presence of anti-CD70 blocking antibody (FR70) or control IgG, and IFN-γ and CD107α expression was analyzed on CD19− CD3− NK1.1+ NK cells by FACS. (F) Numbers of IFN-γ+ NK cells. (G) Numbers of CD107α+ NK cells. (H) Histogram showing the expression of IFN-γ in lymphoma-infiltrating NK cells after PMA/ionomycin restimulation, for 3 tumor samples in each condition. (I) Δ MFI, [MFI-stimulated – MFI-unstimulated], of IFN-γ in Q2A-empty and Q2A-CD27-trunc lymphoma-infiltrating NK cells. Data are shown as mean ± SEM of 3 animals in each group (A-I) and are representative of 3 independent experiments. Statistics: Student t test (A,C-G,I).](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/130/3/10.1182_blood-2016-12-756585/4/m_blood756585f5.jpeg?Expires=1765507166&Signature=kB4HTJ00WQWoXZ44vLotBVBzZWUF8DEIdxNUCAMSPyFLwF0kHTxb0HmV-ne02Lp07HdPDNmNKEFlinx3RwCwVbHukSAmTmIua5FC6uCrGFtOB38GjB0h9tAR58-g0hOzoljnSpZfWq8CZEvu3q~g2kM1s3rdaaE8b5c-NlV~ygnjqAEd5hyXW53qVJWLeTNJT0gD1QzlpMYK3CqfdgKFozE8-kEV56oc6SJY6yQ0CrlC8k8VRam9ibUQHICYeigWtAlnh81gSLDpD3-lJFHKudEjJAhDQpn5zs5PqnjXgZn~ZTr4dp~ZB5N3A1bOjWcARr8VQc8dHHWnJYjBrOHm5Q__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)
![Figure 7. CD70 reverse signaling in human NK cells. (A-B) CD70-negative- CD27-positive- Oci-Ly1 or primary B-ALL cells (patient 1, supplemental Table 1) were cocultured with FACS-sorted CD27-negative NK cells from healthy donors at a ratio of 5:1, in the presence of blocking anti-CD70 antibody or IgG. After 48 hours, IFN-γ and CD107α expression was analyzed. (A) Frequency of IFN-γ+ CD107α+ NK cells. (B) Frequency of Annexin-V+ NK cells. (C-J) Human B-ALL cells (5 × 106; patient 2; supplemental Table 1) were injected IV into NSG mice and analyzed for engraftment in blood at the time points indicated. B-ALL–bearing mice with 5% to 10% engraftment were injected IV with FACS-sorted human NK cells (5 × 106) and treated with anti-CD70 or IgG for 48 hours. (D) Human CD56+ CD3− NK cell numbers in spleens of B-ALL–bearing mice 2 days after NK cell transfer. (E-I) Restimulation of CD19-MACS–depleted splenocytes with PMA/ionomycin. (E-F) Frequencies of IFN-γ+ (E) and IFN-γ+ CD107α+ (F) human NK cells. (G) Δ MFI, [MFI-stimulated – MFI-unstimulated], of IFN-γ in NK cells. (H) Frequency of CD107α+ NK cells. (I) Frequency of Annexin-V+ NK cells. (J) MFI of CD70 on NK cells. Data are shown as mean ± SEM of triplicates per group in panels A-B and 3 animals per group in panels C-J representative of 3 independent experiments. Statistics: Student t test (A-B,D-J). hNK, human NK; PB, peripheral blood.](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/130/3/10.1182_blood-2016-12-756585/4/m_blood756585f7.jpeg?Expires=1765507166&Signature=xqGyBL6ZTwiAnSlNPn4kNjA3H2UbqcZhrdDU3omFd0jlM74vIl5UYzntwXVzuu3sWNCK~B5gWID1R8WPGJRWM2uolyJdNKutbwHS~Z4KBozVBeWloEqvRgbaaZChlmmrp54hxVPZMNuP16evQKwpwWWnQu3yCU-juzJmtSFiJeO89iHCmfVDftrJF2MNsDTbQ2SyATywJSyNv4FBvhraif8EFmXaFgguf516bAL0WgEcwL7hOm2-eo-wxtbfMmcVuzW5ufS97C~z0-CO3AEUjOAeEqK5VjibdZ10eAl-6ajH0rn6b7fYtxDkLKuYDqdnrvL19XQ9pTWyt7XchoqpuA__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)