Abstract
Aggressive NK-cell leukemia (ANKL) represents a rare form of NK cell neoplasm and a distinct disease entity within the continuous spectrum of EBV-T/NK-LPDs. This disease is more prevalent among people from Asia and Central and South America. The median overall survival (OS) is less than two months, irrespective of treatments. Due to the rarity of ANKL, the clinical features and underlying pathogenesis are still lack of understanding.
To date, less than 350 cases of ANKL have been described in English literature worldwide. Most of these cases were sporadic case reports or studies with cohort scales no more than 40 patients. From October 2003 to July 2016, we conducted a retrospective study with 113 confirmed ANKL patients enrolled in 10 clinical centers located in different geographic regions across China. This study was approved by the institutional review board of Tongji Hospital, Tongji Medical College, Huazhong University of Science and Technology. All cases were centrally reviewed by three hematopathologists and three hematologists.
All the patients were of the Han nationality living in the mainland China and had no history of CAEBV, SMBA or other EBV-T/NK-LPDs. Sudden fever, pancytopenia, hepatosplenomegaly, hypofibrinogenemia, hyperferritinemia and elevated lactate dehydrogenase (LDH) levels with dismal survival had characterized in these patients. The median age of the entire cohort was 37 years. The median overall survival was 55 days and 1-year survival rate was 4.42% (5/113). OS was estimated from the onset of disease to the date of death or the end of the study.
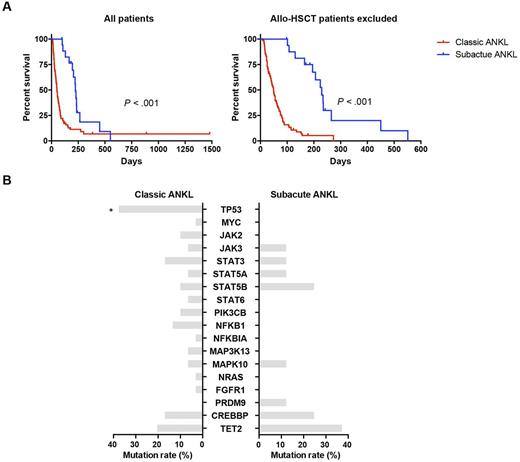
A subacute clinical course was demonstrated in 18 patients (15.93%, 18/113). Prior to the fulminant onset, they manifested infectious mononucleosis (IM)-like symptoms for more than three months (median 4 months, range: 3-15 months). Female predominance (P = 0.007), alleviated hyperferritinemia (P < 0.001), transaminitis (ALT, P = 0.009) and hypofibrinogenemia (P = 0.038) and a marked survival advantage (P <0.001) were noted at diagnosis in these patients, irrespective of whether patients administered with allo-HSCT were excluded or not. Notably, even if the period of prodromal phases were not included in the estimation of the OS of these patients, this marked survival advantage could still be observed when patients received allo-HSCT were excluded (P = 0.042). All these data suggested that patients with prolonged prodromal phases represent a clinical subtype of ANKL which differed with the others. Therefore, we propose to define ANKL with IM-like symptoms lasting for more than 3 months as "subacute ANKL", while the others who had acute clinical course as "classic ANKL".
To clarify the underlying pathogenesis, genes of interest were screened by Ion Torrent AmpliSeq™. The panel contained 18 candidate genes identified in our previous WGS analysis of 8 ANKL patients, including transcriptional factors (TP53 and MYC), JAK-STAT pathway genes (JAK2, JAK3, STAT3, STAT5A, STAT5B and STAT6), other signaling pathway genes (PIK3CB, NFKB1, NFKBIA, MAP3K13, MAPK10, NRAS and FGFR1) and epigenetic regulators (PRDM9, CREBBP and TET2). Our results showed TP53 gene had a significant lower mutation rate in subacute ANKL than that in classic ANKL (P =0.038). Except for that, the other gene mutation patterns including genes in JAK-STAT pathway, were similar between the two groups. Especially, TP53 mutations were not found in patients of subacute ANKL subtype, while enriched in 13 classic ANKL patients (44.83%, 13/29). In addition, most of the detected TP53 missense mutations (61.54%, 8/13) were located in the DNA binding domain.
Survival analysis revealed L-asparaginase, methotrexate and dexamethasone (AspaMetDex) was an effective induction regimen with no therapy-related mortality. The complete remission rate and overall response rate in newly diagnosed patients was 30.77% (4/13) and 76.92% (10/13), respectively. Allo-HSCT was the only curative treatment with 2-year survival rate of 43.86% (3/7). Multivariate analysis showed serum LDH level, clinical subtype and administration of L-asparagine based chemotherapy or allo-HSCT were factors independently predictive for survival.
In conclusion, these data depicted the clinical characteristics and molecular features of ANKL. It also provided insights into the treatments and outcomes of this deadly type of leukemia. Future prospective studies or clinical trials hold great promise for ANKL.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.