Abstract
Background: For patients with beta-thalassemia major (TM), the optimization of both blood-transfusion and iron-chelation has resulted in a remarkable improvement in the life expectancy and the gene therapy has showed a good prospect,however, only allogeneic hematopoietic stem cell transplantation (HSCT) currently remains a curative therapy. Although experiences on leukemia proved that HLA matched alternative-donor transplant (MAT), including matched unrelated-donor transplant (MUT)and matched parent-donor transplant MPT), had similar outcomes as matched sibling transplant (MST), a large-cohort multicenter TM-MAT study has not yet been reported.Hence, we designed the current study.
Methods: 583 consecutive TM-patients from four pediatric centers in China underwent HSCT between Jan. 2009 and Jun. 2016, with median follow-up time of 46 months (range: 10-105 months). Rate of male to female was 376:207. The median age at transplant was 6 years (rang:1-23years). Of them, 314 patients received MAT consisted of 235 HLA 10/10 (full-match) MAT (F-MAT) and 79 HLA 9/10 (well-match) MAT (W-MAT), and 269 patients received MST adopting bone marrow and/or cord blood. Among MAT, 214 received F-MUT and 60 W-MUT, and 21F-MPT and 19W-MPT. All patients received the NF-08-TM protocol (see Li et al., Blood 2012) briefly composed of Cyclophosphamide (Cy), IV Busulfan (by age-dependent dose adjustment and following Cy), Fludarabine and Thiotepa. Prophylaxis of GVHD consisted of ATG, Cs A, MMF and short MTX.
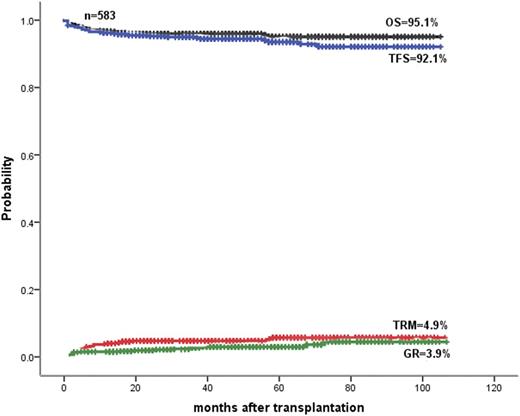
Results: The estimated 5-year overall survival (OS), TM-free survival (TFS), cumulative incidence of graft rejection (GR) and cumulative transplant related mortality (TRM) in total were showed on the Figure. OS and TFS were 93.3%,and 91.8%,and 97.4% and 96.2% in MAT and MST, respectively. GR and TRM were 3.1% and 1.7%, and 6.7% and 2.6% in MAT and MST, respectively. Acute GVHD, chronic GVHD, venous occlusive disease and hemorrhagic cystitis were 18.6%,4.1%, 1.2% and 12.7%, and 9%, 2%, 4.3% and 6.9%, respectively, in MAT and MST.Acute GVHD (18.6% vs. 9%, P=0.001) and cytopenia (18.1% vs. 7.5%, P=0.002) in MAT was more than MST. Although no significant differences were found in comparison of F-MAT with W-MAT in OS (93.4% vs. 92.3%,P=0.487), TFS (89.1% vs. 90.9%,P=0.876), TRM (6.6% vs. 7.7%,P=0.487) and GR (5.6% vs. 4.2%,P=0.545), cytopenia post-transplant in W-MAT was more than F-MAT (27.4% vs. 15.1%, P=0.022).
Conclusion: The current large-cohort multicenter TM-MAT prospective study showed that MAT had comparable result as those from MST for TM patients receiving NF-08-TM protocol. Despite similar OS and TFS, F-MAT is superior to W-MAT for TM-patients because the latter has more the complication than the former.
Fig. OS, TFS, TRM and GR in 583 HSCTs in patients with beta-thalassemia major
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.