Abstract
Introduction. The incidence of immune thrombocytopenia (ITP) in adults increases with age. Aging, through comorbidities, polymedication, impaired functional capacities may further increase the severity of ITP and reduce the therapeutic landscape. With the aging of the population, the number of elderly ITP pts will continue to rise in parallel. However, limited data are available in this specific pts population.
Aims. To report the impact of age on treatment strategy and clinical outcome of elderly ITP pts .
Methods. Based on an internal database including over 800 ITP pts, we analysed data on 508 ITP patients diagnosed between 1995 and 2017 at the "Seràgnoli" Institute of Hematology, Bologna, Italy. Treatment decisions were at the physician's discretion. Diagnosis and responses were assessed according to current guidelines and terminology. Infectious, thrombotic and hemorrhagic complications were graded according to the WHO scale. Numerical variables have been summarized by their median and range, and categorical variables by count and relative frequency (%) of each category. Association between categorical variables (2-way tables) was tested by χ2. Survival curves were calculated by the Kaplan-Meier method from the date of ITP diagnosis to the date of first appearance of the event. Event-free survival (EFS) include infections, thrombosis, hemorrhages and death. Survival curves of different subgroups were compared by the log-rank test. All statistical analyses were computed with STATA software.
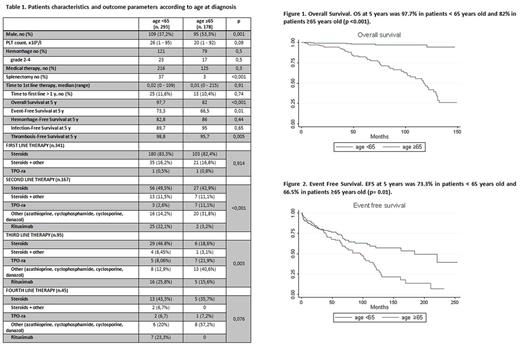
Results. A total of 508 consecutive ITP pts were included in the analysis and were sub-grouped according to older age at diagnosis (≥65 yrs). Baseline characteristics of the total population were: median age: 56 yr (16-95); median platelet count: 23 (1-95); number of pts with hemorrhages: 200 (42.7%, grade 3-4: 6%). 341 pts (67.1%) received a front-line therapy for ITP after a median time from diagnosis of 0.1 mos (0-215); 152 (44.6%) started therapy in chronic phase (CP) (Table 1).
A second-line approach was required in 167 pts (49%) while 95 (27.8%) patients received also a third-line therapy; 45 and 18 pts required 4 and >4 treatment therapies, respectively. Median follow-up was 35.7 mos (1-254). 54 (10.6%) patients died; death was due to major hemorrhage in severe thrombocytopenia in 1 case. A total of 12 thromboses, 114 bleedings and 63 infections were observed. Incidence rate of ≥G2 complications were: 0.49% pt-yr (thrombosis), 3.8% pt-yr (hemorrhages); 1.82% pt-yr (infections).
Kaplan-Meier analysis of outcome parameters showed that elderly pts had a significantly worse overall survival, event-free survival and thrombosis-free survival compared to younger pts (Figure 1-2). Notably, the hemorrhage and infection-free survival was comparable in the two cohorts.
The proportion of male over female ITP pts progressively increased along with older age, being 23% for pts aged<40 yr and reaching 50% when aged>65 yr. Consequently, compared to younger pts, elderly pts were more frequently males; baseline features and treatment requirement were comparable (Table 1). Notably, while the type of front-line treatment was comparable across age groups, the percentage of pts achieving a complete response (CR) was significantly lower in the elderly, probably due to lower intensity (duration and dose) of corticosteroids treatment. Second-line, prednisone (PDN)/PDN combination was less frequently used in the elderly, that were preferentially treated with Thrombopoietin-receptor agonists (TPO-ra) (70% vs 30%). Conversely, rituximab (RTX) and splenectomy were the most frequently used second-line therapies in younger pts. Third line, while younger pts were mostly treated with RTX, the elderly received mild immunosuppressive agents (e.g. azathioprine, cyclosporine A). At last contact, 57.1% pts were in CR, 37.3% were in Response and 5.6% had no response (NR), with no significant differences between the two groups.
Discussion. This analysis demonstrates that aging is a crucial factor in second-line decision making in a real-life setting in ITP. The use of less immunosoppressive therapies may have reduced the incidence of infectious events, while the higher rates of thromboses observed in the elderly could be due to age-related factors rather than intrinsic ITP factors. Prospective clinical trials investigating age-adapted treatment strategies should be further explored in elderly ITP pts.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.