Abstract
Background: Multiple myeloma (MM) is consistently preceded by monoclonal gammopathy of undetermined significance (MGUS), but a clinical diagnosis is only made in a small proportion of patients prior to the MM diagnosis. In a smaller proportion of patients, there is a preceding diagnosis of smoldering myeloma (SMM) or plasmacytoma (PC) as well. Prior studies have suggested a better outcome for MM patients with a pre-existing diagnosis of MGUS, but there is a paucity of data analyzing the potential reasons for this, as well as impact of prior SMM and PC on MM outcomes.
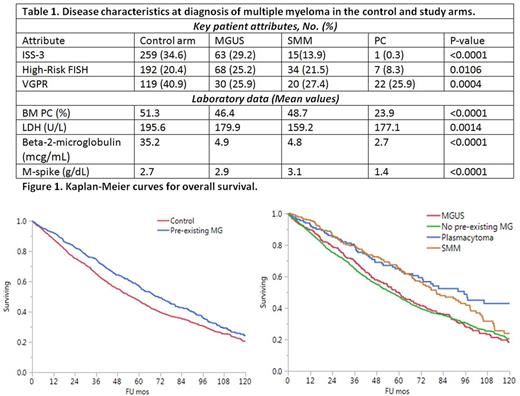
Patient and methods: Patients with prior diagnosis of MGUS, SMM or PC from 1973 to 2015 were identified from our institution's database. We selected a control cohort (1:2) of patients who had MM without prior diagnosis of MGs that was matched for the year of diagnosis. Descriptive statistics are depicted as medians with inter-quartile range (IQR) or frequencies. Comparison of variables between individual groups was conducted using t-test, or Wilcoxon rank sum test, and contingency analysis. Overall survival (OS) was calculated using Kaplan-Meier method and compared using Log-Rank test.
Results: We identified 774 patients with a prior diagnosis of MGUS, SMM or PC (cases) and a control population (1:2) matched for the year of diagnosis (n=1,548). The case cohort distribution was as follows: MGUS 407, SMM 232, and PC 135. The median age at diagnosis of MM in the case cohort was 66.2 years (IQR 58-72) and for the control cohort was 62.9 years (IQR 55-70); gender distribution was similar. Among the cases, pre-existing MGUS patients were older (median age 68.4 years) as compared to SMM (64 years) and PC (61.3 years) patients. After a median follow-up of 80.8 months, the cases showed better OS than the control group (70.6 vs. 55.5 months), (Figure 1). Further analysis of the study group showed that better survival was limited to those with a prior diagnosis of SMM (80.3 months) and PC (95.4 months), compared to MGUS (59.8 months). The depth of response to first line treatment (VGPR) was lower in the patients with pre-existing MGs as compared to the control group (31.7% vs. 40.9%, P=0.03). The control group had higher proportion of bone marrow plasma cells (BM PC %), LDH levels, and beta-2 microglobulin as compared to patients with pre-existing MGs (Table 1). Further, prior SMM and PC group had lower proportion of high-risk (ISS-3) patients as compared to the MGUS and control group.
Conclusion: Our study shows that MM patients with pre-existing MGs had superior outcomes as compared to those without. Specifically, prior SMM and PC diagnosis was associated with a better MM prognosis as compared to prior MGUS patients. This could be related to less proportion of SMM and PC patients with advanced stage (ISS-3) disease, lower LDH levels, lower beta-2 microglobulin, thereby suggesting lesser tumor burden and potentially earlier intervention in these patients who are followed closely. This is in contrast to patients with prior MGUS, where the follow-up is less often, and has not been shown to prolong survival and/or prevent MM complications. It may also reflect, a more prolonged duration of the precursor state thus facilitating its clinical discovery, suggesting a more indolent biology.
Gertz: Millennium: Consultancy, Honoraria; Celgene, Novartis, Smith-Kline, Prothena, Ionis, Amgen: Honoraria. Dispenzieri: Celgene, Millenium, Pfizer, Janssen: Research Funding. Russell: Imanis Life Sciences: Equity Ownership; Vyriad: Equity Ownership. Kapoor: Takeda, Celgene and Amgen: Research Funding. Kumar: Celgene, Millennium/Takeda, Onyx, AbbVie, Janssen, Sanofi, Novartis, Amgen, Genentech, Merck, Oncopeptides, Roche, Skyline Diagnostics: Research Funding; Celgene, Millennium, BMS, Onyx, Janssen, Noxxon, AbbVie, Amgen, Merck, Oncopeptides, Skyline Diagnostics, Takeda: Consultancy; Skyline: Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.