Abstract
Introduction
High dose melphalan 200mg/m2 (MEL200) followed by autologous stem cell transplantation (ASCT) is the standard of care for fit patients with Multiple Myeloma (MM). Bendamustine has been shown to induce responses in MM resistant to other alkylating agents. Our prior Phase I trial, adding bendamustine to MEL200, demonstrated no additional toxicity above that expected with MEL200 alone (Mark et. al. BBMT 2013). A phase 2 trial of bendamustine/MEL200 conditioning was conducted to evaluate treatment efficacy.
Objective and Methods
This single arm, open-label, phase II study was designed to establish the efficacy of Bendamustine (225 mg/m2) in combination with MEL200 in patients undergoing first ASCT for MM. Patients 18 to 75 years with confirmed MM, prior induction therapy, adequate mobilization (at least 2x106 of CD34+ hematopoietic stem cells), Karnofsky performance status >70% and life expectancy >12 weeks were eligible for screening. Major exclusion criteria included serious/uncontrolled medical conditions, or previous ASCT. Responses were determined according to the IMWG response criteria and adverse events (AEs) were reported per CTCAEv4.0. The primary endpoint was to evaluate the overall response rate (ORR) and CR or better at 6 months.
Results
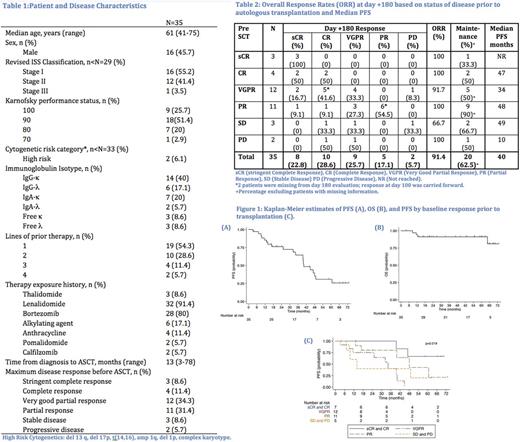
A total of 35 patients were enrolled (Table 1). Median age was 61 (range 41 - 75). Intermediate or high-risk disease was present in 44.8% by R-ISS. All patients engrafted. Median time to neutrophil and platelet engraftment was 11 days (range 10-14) and 21 days (range 15 to 29) respectively. At day +180, the ORR was 91.4% and 51.4% of patients achieved a CR or sCR (Table 2). Only 1 patient progressed before day +100 (R-ISS 1 double-refractory to lenalidomide + bortezomib, achieved VGPR with second line therapy with VDT-PACE prior to transplant), and one additional patient progressed before Day +180 (R-ISS 2, with prior 4 lines of therapy, SD prior to transplant). Maintenance was initiated in 20 patients out of 32 patients (62.5%). Choice of maintenance was at the discretion of the treating physician and patient.
After a median 33 months (range 3-73) of follow up post ASCT, 20 patients had progressed (57.1%), 4 of whom died from complications of MM progression (11.4%). Median progression free survival (PFS) was 40 months (14 months vs 48 months depending on maintenance therapy, p=0.024). The 3 year PFS was 64.5% (95%CI 44.7-78.8). The median overall survival (OS) was not reached. The 3 year OS was 91.2% (95%CI 75.1-97.1) (Figure 1). Baseline response, categorized as CR or better, VGPR, PR and SD or PD prior to transplant, was statistically significant for PFS (p=0.019). In a multivariable Cox proportional hazards model controlling for baseline response prior to transplant, maintenance therapy continued to be associated with improved PFS (HR 0.16, p=0.004). No variable had a statistically significant impact on OS. There was no transplant related mortality (TRM). The most common overall AEs were hypocalcemia (100%), nausea (94.3%), fatigue (94.3%), anorexia (91.4%), mucositis (57.1%), abdominal pain (51.4%), peripheral edema (48.6%) and constipation (34.7%). The most frequently observed grade 3 AEs were febrile neutropenia in 45.7% of patients, hypocalcaemia in 34.3%, hypokalemia in 20%, and hypophosphatemia in 14.3%. There was only one grade 4 AE, hyperbilirubinemia associated with a reaction to antibiotics.
Conclusion
We confirmed that Bendamustine can safely be combined with standard dose MEL200 as a conditioning regimen for ASCT. This regimen shows promising efficacy, with median PFS of 48 months for patients who received maintenance. Further evaluation of this conditioning regimen in a Phase III comparison trial with single agent MEL200 is warranted in conjunction with newer induction approaches and standard maintenance therapies. (NCT00916058).
Niesvizky: Celgene: Consultancy; BMS: Consultancy; Amgen: Consultancy; Janssen: Consultancy. Rossi: Celgene: Consultancy; Thrassos: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.