Abstract
Background
Multiple myeloma (MM) is a monoclonal B-cell malignancy with a terminally differentiated plasma cell phenotype and monoclonal immunoglobulin production and subsequent end organ damage. Current treatment paradigm includes autologous hematopoietic stem cell transplant (ASCT) after initial induction with combination doublet/ triplet therapy. While complete response (CR) is ideal as it correlates to improved OS, many patients undergo ASCT in VGPR or PR. Previous studies have suggested that rapid reduction in serum free light chains in response to chemotherapy may be representative of a poorly differentiated clone and hence may carry a worse prognosis. We evaluated free serum light chain response of pts with MM in VGPR or PR after ASCT to determine its impact on post ASCT outcomes.
Methods
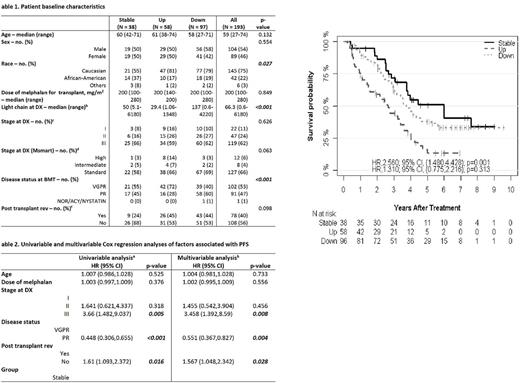
After obtaining Wayne state university institutional review board approval, we retrospectively studied pts with MM in PR or VGPR who underwent first ASCT at out institution between Jan, 2002 to Jan, 2012. Data was collected on baseline demographics, ISS stage at diagnosis, cytogenetics at diagnosis, light chain and M spike at diagnosis, date of transplant, melphalan dose, light chain and M protein at diagnosis, just prior to transplant (0), 3, 6 and 12 month after ASCT and post transplant maintenance lenolidomide use. Responses after induction were assessed using IMWG response criteria. Post ASCT, pts were grouped based on the light chain responses ('Up' if relative change ≥25% increase, 'Down' if >25% decrease, and others as "stable"). We also assessed response with M protein using same criteria. OS was calculated as the time from the date of transplantation to death from any cause. Patients, who were alive, were considered censored at the date of last observation. PFS was calculated as the time from the date of transplantation to the date of progression (based on IMWG criteria or need for restarting therapy) or death from any cause. Univariable and multivariable Cox proportional hazards regression models were fit to assess associations between six prior chosen predictors (age, dose of melphalan, stage, disease status, post-transplant len, and light chain response postASCT) and survival benefit (PFS and OS).
Results
We identified 231 pts who underwent AutoSCT; 193 pts (84%) had follow up data for 1 yr and were included. There were 104 (54%) male pts and 145 (75%) were Caucasian. 95% had one line of therapy prior to ASCT and 102 (53%) were in VGPR. Median time to transplant was 7.54 months .Post ASCT 38 pts had stable response by light chain criteria(21 VGPR, 17 PR), 58 pts up (42 VGPR, 28 PR) and 97 down (39 VGPR and 91 PR. M protein values were available for 153 pts and consensus analysis of the 3 clusters with both light chain and M peak values significantly concordant (p = 0.003) Forty percent of all pts received post-transplant len maintenance. PFS in the 'stable' and 'down' gps were similar (HR 1.31, 95%CI 0.78-2.21 p=0.31). OS was significantly improved in 'stable' vs 'down' gp (HR2.77 (95% CI 1.26-6.11; p=0.01). On multivariate analysis, post-transplant len was associated with increased PFS (HR 1.57; 95CI 1.05-2.34 p=0.03) and OS (HR 1.96; 95 CI 1.14-3.36, p=0.01)
Conclusion
ASCT following induction chemotherapy is currently the standard therapy for eligible MM pts. While response to induction therapy has been prognostic, impact of continued response post ASCT is unclear. We demonstrate that light chain response post AutoSCT correlates with M protein and can be used as a marker to assess response post-ASCT. In our cohort, patients with stable serum light chains / M-spike post ASCT had at least equivalent outcomes to patients who had further decrease in their serum markers. Post ASCT len maintenance was found to be associated with improved PFS and OS.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.