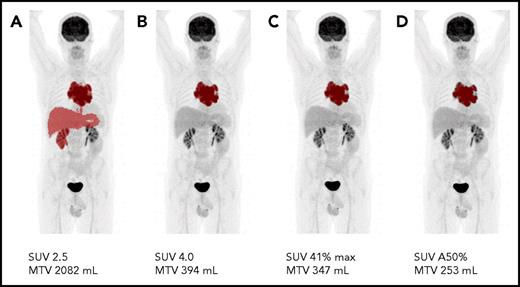
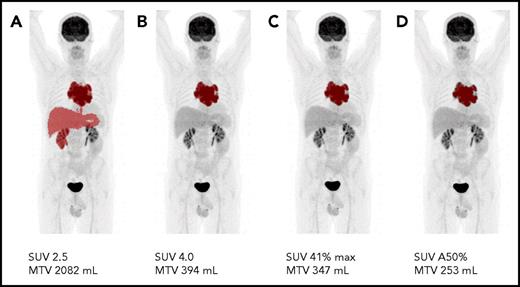
Metabolic tumor volume measured with different cutoff values. (A) Example of a clearly failed MTV delineation when using the SUV 2.5 delineation method for this specific patient study. Even visually similar and accurate tumor volumes (B-D) are quantitatively substantially different.
Metabolic tumor volume measured with different cutoff values. (A) Example of a clearly failed MTV delineation when using the SUV 2.5 delineation method for this specific patient study. Even visually similar and accurate tumor volumes (B-D) are quantitatively substantially different.
HL is a highly curable malignant lymphoma and often affects young adults. Personalized PET-guided treatment is currently the focus of many large international trials, mainly to diminish early and late toxicity of treatment, while maintaining the relatively good outcome. Accurate staging is of utmost importance to select the appropriate treatment regimen, currently consisting of 2 to 4 cycles of doxorubicin, bleomycin, vinblastine, and dacarbazine (ABVD) plus radiotherapy for early-stage HL, and chemotherapy only (6-8 cycles of ABVD or 4-6 cycles of BEACOPP [bleomycin, etoposide, doxorubicin, cyclophosphamide, vincristine, procarbazine, prednisone] escalated) for advanced-stage HL. With the introduction of PET using 18F-fluorodeoxyglucose (FDG) in the mid-1990s, and PET-CT (with low-dose unenhanced CT) in the last decade, it became clear that metabolic imaging not only created a new tool for assessment of response during and after treatment, but also provided the possibility of quantifying tumor load and accurately assessing volumetric tumor burden.
Akhtari and colleagues describe a cohort of 267 patients with stage I to II HL (diagnosed between 2003 and 2013) whose pretreatment PET-CT scans of MTV was assessed using manually contoured volumes and by using standardized uptake values (SUV) thresholds. Tumor volumes, defining bulky masses, were correlated to progression-free survival and overall survival and seemed to discriminate between low- and high-risk disease, enabling risk stratification in early-stage unfavorable HL patients.
However, what is the definition of bulky disease? Until now, one of the most striking differences between favorable and unfavorable early-stage HL is the presence of a bulky mass. However, there have been inconsistency and confusion with respect to the definition of “bulky disease.” The European Organization for Research and Treatment of Cancer and German Hodgkin Study Group define bulky disease as a mediastinal mass ratio of >0.35 and 0.33, respectively, using conventional radiograph of the thorax. Otherwise, the National Comprehensive Cancer Network and National Cancer Institute of Canada are also using a 1-dimensional measurement of lymph nodes >10 cm (using CT scanning) as a definition of bulky disease. This definition is more comprehensive because a bulky mass is not always located in the mediastinum. According to the Lugano classification,3,4 staging for HL has to be performed using PET-diagnostic CT scanning. Therefore, it would be reasonable to use PET-CT for the determination of bulky disease. The retrospective analysis from Akhtari and colleagues is a major step forward in that direction.
However, the cutoff values mentioned in this publication must be assessed with caution. These values are derived from a single-institution and a retrospective dataset. The authors emphasized that validation of these findings, with PET-CT scans obtained using a standardized approach, is essential.
In recent years, the guidelines for standardization of PET-CT scanning for oncologic studies have been performed by hematologists, nuclear medicine physicians, and clinical physicists from Hemato-Oncology Foundation for Adults in the Netherlands,5 the European Association of Nuclear Medicine, and the Society of Nuclear Medicine.6,7 These guidelines were designed to achieve SUV consistency for multicenter settings, that assist physicians in performing, interpreting, and reporting the results of PET-CT. For example, the interval between injection and start of scanning (60 vs 90 minutes) will influence the quantification of FDG uptake and thereby also the MTV measurement. Therefore, image quantification needs to be standardized also regarding the reconstruction methods and settings used.
Another important issue is the contouring of MTV. There is no universal consensus on how to define and assess MTV.8 Several absolute and relative thresholds have been suggested, and none of these has proven consistently superior to the others, as Akhtari and colleagues correctly state. To illustrate these differences, 1 PET-CT scan has been analyzed with different commonly used MTV contouring methods (cutoff SUV 2.5; SUV 4.0; SUV 41%max; SUV A50%), resulting in a range of MTVs from 253 mL to 2082 mL (see figure).
Akhtari and colleagues have performed an accurate and significant analysis of baseline PET-CT characteristics in early-stage HL. Moreover, they have raised the critical issues of the definition and importance of bulky disease. However, an individual patient data meta-analysis based on results of prospective clinical trials in HL is needed to solve the above-mentioned issues that still exist with regard to the contouring of MTV. For implementation in daily practice and for use in clinical studies, a semiautomated, reliable, and easy-to-use contouring method is needed.
We conclude that, in HL, the MTV as baseline characteristic seems of additive value in risk stratification. However, standardization of PET-CT scanning has to be implemented, and definition of MTV measurement procedures has to be settled before MTV can be used for clinical decision-making.
For daily practice, the interim-PET in correlation with baseline PET is important because chemosensitivity is mainly reflected by interim-PET assessment. Recent publications in early- and advanced-stage HL have emphasized the predictive value of interim-PET using visual assessment.9,10 The relationship between baseline MTV and interim-PET assessment, visually or by using semiquantitative parameters, is intriguing and the subject of ongoing studies. It is most likely that, in the near future, baseline characteristics as well as interim-PET–adapted treatment strategies will enhance individually designed and tailored therapy, supporting maximal efficacy and minimal toxicity!
Conflict-of-interest disclosure: The authors declare no competing financial interests.