In this issue of Blood, Chapman et al1 have derived a 7-gene expression signature that predicts whether a newly diagnosed myeloma patient will respond to treatment with bortezomib when autologous stem cell transplant (ASCT) is not considered as part of the upfront therapy.
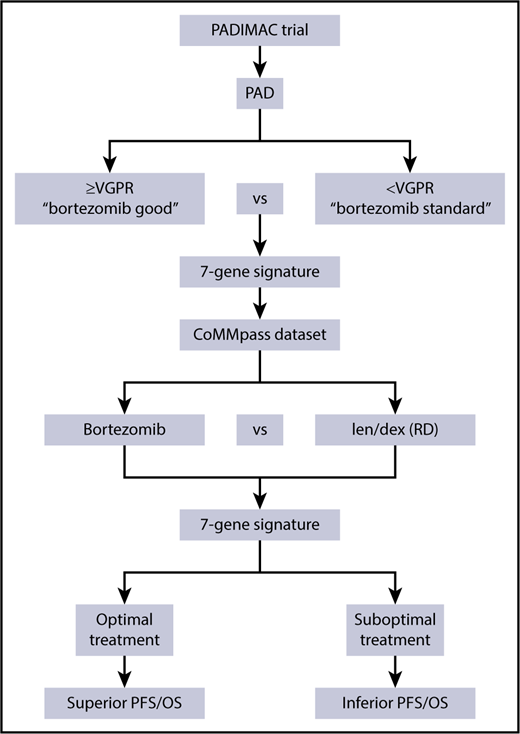
Overview of the process to generate and validate a RNA-seq gene signature to determine optimal treatment. CoMMpass, Clinical Outcomes in Multiple Myeloma to Personal Assessment of Genetic Profile; OS, overall survival; PAD, bortezomib, adriamycin, and dexamethasone.
Overview of the process to generate and validate a RNA-seq gene signature to determine optimal treatment. CoMMpass, Clinical Outcomes in Multiple Myeloma to Personal Assessment of Genetic Profile; OS, overall survival; PAD, bortezomib, adriamycin, and dexamethasone.
The goal of the phase 2 PADIMAC (Bortezomib, Adriamycin, and Dexamethasone Therapy for Previously Untreated Patients with Multiple Myeloma: Impact of Minimal Residual Disease in Patients with Deferred ASCT) trial is to provide a reliable estimate of the 2-year progression-free survival (PFS) in patients achieving very good partial response (VGPR) or better to induction therapy with bortezomib, adriamycin, and dexamethasone. RNA was isolated and sequenced from patients in the trial from CD138+ sorted cells from bone marrow aspirates. To ensure the robustness of the data set, the team performed several quality control checks on the sequencing data for expected myeloma characteristics including expression of key translocation partner oncogenes, presence of expressed mutations, and fusion genes between immunoglobulin and MMSET.
The 44 patients in the study were classified by response, where those with a VGPR or better and who were progression-free at 1 year without ASCT were classified as “bortezomib-good”; the remaining patients were “bortezomib-standard” (see figure). Comparison of the 2 groups identified an optimal 7-gene signature, consisting of EMC9, FAM171B, PLEK, MYO9B, RCN3, FLNB, and KIF1C. Three of these proteins are associated with the endoplasmic reticulum, 3 associated with actin filaments, and probably most important, 3 (EMC9, MYO9B, and KIF1C) are positively associated with proliferation.
To ensure that the signature was robust, the authors used it to determine its predictive power in a separate data set, namely a subset of the CoMMpass data set. This data set consisted of previously untreated patients who did not proceed to ASCT, who were either treated with bortezomib (without an immunomodulatory drug, n = 147), with lenalidomide and dexamethasone (RD) (n = 40), or both (n = 208). The 7-gene signature was used to identify patients within the CoMMpass study who would benefit from bortezomib-based therapy, and indeed, those who were assigned to the “bortezomib-good” group had a better PFS.
The most important finding of the group was to show that patients predicted to do well with bortezomib actually have an inferior PFS when treated with RD and vice versa. Therefore, in future prospective studies, it may be important to assign treatment regimens based on their gene expression profiles at diagnosis. To test this hypothesis, the authors used the data set to determine which patients should have received either bortezomib or RD, based on the 7-gene signature, and compared the outcome of patients who received the correct treatment. This showed that those with the correct predicted treatment had a superior PFS and overall survival.
Gene expression profiling has been used in myeloma for more than a decade to determine high-risk subgroups, translocation subtypes, proliferation rates, and prognostic subgroups.2-6 It is increasingly important when treating patients to be able to identify the most effective, cost-efficient regimen with the fewest toxicities. In this regard, precision medicine has been used to identify subgroups of patients with genomic abnormalities to receive treatments directed against the identified abnormality. Here, however, the authors have shown using RNA-sequencing that it is possible to predict which treatment will result in a superior response when considering novel agents that are not targeted against specific genomic abnormalities. This methodology could be used for other drug combinations to further identify optimal treatments for patients, including those undergoing transplants.
Conflict-of-interest disclosure: The author declares no competing financial interests.