Abstract
Sickle cell disease (SCD) is an inherited red blood cell disorder that leads to substantial morbidity and a heavy burden on the health care system. Nonmyeloablative allogeneic hematopoietic stem cell transplantation (HSCT) regimens using HLA-matched related donors have recently demonstrated high rates of engraftment and a favorable safety profile in adults with SCD. The long term effects of these HSCT regimens on health care utilization, particularly in SCD adults who have had a high burden of SCD-related acute and chronic complications, has not been previously reported.
Between 8/2011 and 4/2016, 86 SCD patients who received their routine care at our institution were referred to the Blood & Marrow Transplant Clinic. Sixteen patients received a HSCT from an HLA-match related donor during this time period. Reasons for not proceeding to transplantation in the 70 patients included lack of an HLA-matched related donor in 36 (51%), patient/family declining in 21 (30%), insurance denial in 11 (16%), and the presence of RBC antibodies to potential donors in 2 (3%) patients. We compared health care utilization patterns between 1) 1-year pre-HSCT vs. 1- and 2-years post-HSCT in 16 transplanted SCD adults and 2) 16 transplanted vs. 70 non-transplanted SCD patients at 1- and 2-years from the time of HSCT or referral. Comparisons of linear variables and categorical variables were performed using the Kruskal-Wallis and Chi-square test, respectively.
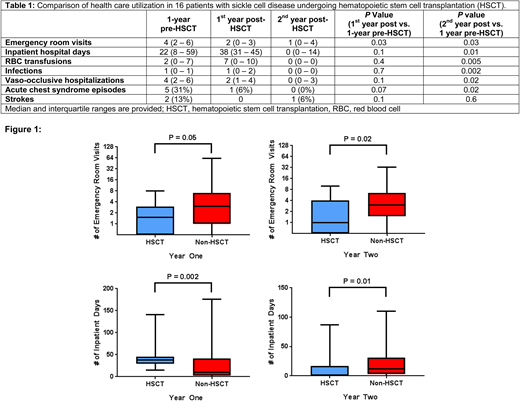
In the 16 SCD patients who met standard transplant eligibility criteria and underwent HSCT, the median age at the time of HSCT was 33 years (interquartile range [IQR], 24 - 34 years), 56% were male, and 94% were HbSS genotype. Treatment prior to HSCT was hydroxyurea in 10 (63%), chronic red blood cell (RBC) transfusion therapy in 5 (31%), and no disease modifying therapy in 1 (6%) patient. Thirteen of 16 (81%) transplanted SCD patients maintained a stable graft. Emergency room (ER) visits were lower 1-year and 2-year post-HSCT compared to 1-year pre-HSCT (P=0.03) (Table 1). In the 2nd year post-HSCT, ER visits, hospital length of stay, RBC transfusion requirements, and rates of documented infections were all lower compared to 1-year pre-HSCT (P<0.03).
We then compared health care utilization patterns between the 16 SCD patients that underwent HSCT vs. the 70 SCD patients that were not transplanted. The HSCT and non-HSCT patients were similar with respect to median age (33 vs. 31 years old; P=0.2), gender (35% vs. 56% male, P=0.1), number of eligibility criteria met for HSCT (PMID: 24319206) (2 for each group; P=0.4) and SCD genotype (80% vs. 94% HbSS genotype, P=0.4), respectively. During the first year after transplant or of observation, we observed lower rates of emergency room visits but a greater number of inpatient hospital days in the HSCT vs. no HSCT groups (Figure 1). During the second year, both the number of emergency room visits and the number of inpatient hospital days were lower in the HSCT vs. the no HSCT patients (Figure 1).
In conclusion, we demonstrate that allogeneic HSCT leads to lower health care utilization by the second year post-HSCT in adults with SCD. These results support the role for HSCT to lower the morbidity, health care burden and costs associated with SCD and should encourage universal insurance coverage for HSCT in adults with SCD.
Patel:Celgene: Consultancy, Honoraria; Amgen: Consultancy, Honoraria; Janssen: Honoraria. Khan:Teva: Speakers Bureau.
Author notes
Asterisk with author names denotes non-ASH members.