Abstract
BACKGROUND: Recipients of allogeneic HSCT experience significant short- and long-term healthcare burdens with differing general patterns of late effects between graft sources. For example, recipients of peripheral blood stem cell (PBSC) grafts benefit from more rapid engraftment after transplant as compared to bone marrow (BM) or umbilical cord blood (UCB), but experience a greater risk of chronic graft-versus-host disease (cGVHD) at later time points after HSCT. Little data exist regarding healthcare burden beyond first year of allogeneic HSCT, limiting our understanding of the long-term impact for each graft source.
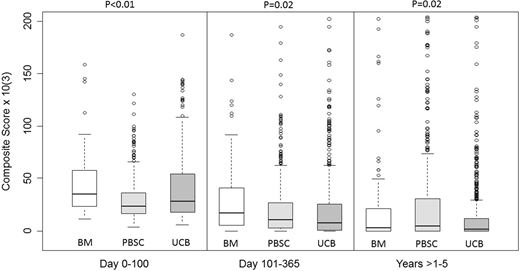
METHODS: To estimate the healthcare burden in adult allogeneic HSCT recipients over time, we analyzed clinical data from 1077 consecutive allogeneic HSCT recipients at the University of Minnesota Medical Center (UMMC) transplanted between 2000-2016. In order to understand changes in healthcare burden over time, we assessed the raw number of visits (both face-to-face and non-face-to-face care coordination visits), procedures, laboratory studies, medications, and relative value units (RVUs) over 3 time periods: (1) Day 0 to day 100, (2) 101 - 365 days, and (3) >1 year - 5 years after HSCT. We analyzed the counts of these healthcare elements both individually and as a composite score of all these elements (visits, procedures, labs, medications, RVUs). We then compared the estimated healthcare burden by graft source over each time period. We included only patients undergoing their first allogeneic HSCT in this analysis, and we included all clinical data from transplant to death or 5 years, whichever came first. We retained data from patients experiencing post-HSCT relapse in this analysis.
RESULTS: Of the 1077 HSCT recipients, 102 received BM, 458 received PBSC, and 517 received UCB (84.7% double). The majority of BM donors were matched but unrelated to the recipient (57%), and the majority of PBSC donors were matched siblings (88%). The median age was 52.2 years (range 18.1 - 75.1 years), and 41.4% of the patients were female. The median distance from the patients' address to the transplant center was <30 miles, with no significant difference between the graft sources at any of the 3 time periods (p=0.12, p=0.10, p=0.09, respectively). The majority of patients had acute myeloid leukemia (40.8%), acute lymphoblastic leukemia (13.7%), non-Hodgkin lymphoma (13%), and myelodysplastic syndrome (12.8%). There was no significant difference in the proportions of patients with death (p=0.50) or relapse/progression (p=0.22) between graft sources over these time periods. As expected from previous data, recipients of PBSC had the lowest median composite healthcare burden in the first 100 days (p<0.01, Figure). During this earliest time period, the median number of laboratory studies (2,213 vs 2,448.0 vs 2,960, p<0.01), medications (132 vs 232 vs 203, p<0.01), and RVUs billed (423.2 vs 480.7 vs 466.7, p<0.01) were significantly lower for recipients of PBSC vs BM vs UCB respectively, with no difference in number of visits (p=0.07). From day 101 - 365, UCB had the lowest composite score (p=0.02) due to the fewest labs and visits performed (p<0.01 for each). There was no difference between medications (p=0.16) or RVUs (p=0.06) between graft sources in this second time period. Beyond 1 year, UCB continued to have the lowest composite score (p=0.02), with the lowest number of visits (p<0.01), labs (p<0.01), procedures (p=0.03), medications (p<0.01), and RVUs (p=0.02) with this graft source compared to BM and PBSC.
CONCLUSION: Adult recipients of UCBT appear to experience a lower long-term healthcare burden compared to other graft sources. After the first year post-HSCT, recipients of UCBT have fewer clinic visits, laboratory tests, procedures, and medications. This study is the first step in analysis of complex, long-term healthcare burden data in allogeneic HSCT recipients within a single healthcare system. Despite the absence of cost data and details of care outside of Fairview, these data support the hypothesis that healthcare burden varies by graft source with favorable outcomes in long-term survivors after UCBT compared recipients of BM and PBSC.
Brunstein:Gamidacell: Research Funding. MacMillan:Angiocrine: Membership on an entity's Board of Directors or advisory committees; CSL Behring: Consultancy; Equillium: Consultancy. Wagner:Novartis: Research Funding; Magenta Therapeutics: Consultancy, Research Funding. Weisdorf:SL Behring: Consultancy; Seattle Genetics: Consultancy; Pharmacyclics: Consultancy; FATE: Consultancy; Equillium: Consultancy. Holtan:Incyte: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.