Abstract
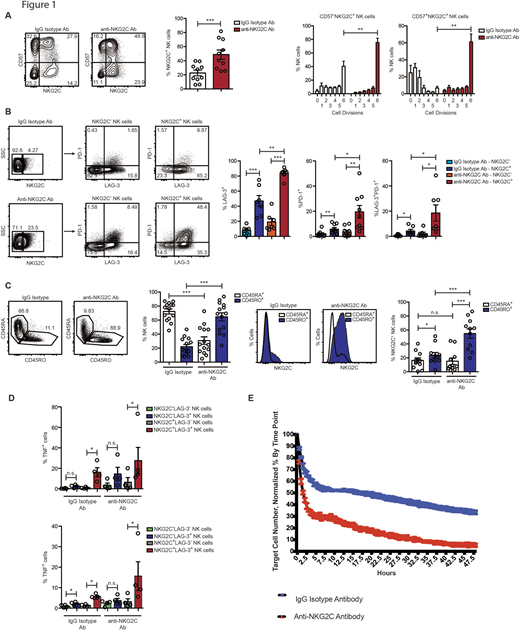
Natural killer (NK) cells can eliminate myeloid leukemia cells after stem cell transplant, yet many patients relapse. Several reports have described significant decreases in relapse rates post-transplant in recipients that experienced cytomegalovirus (CMV) reactivation. Our group has shown that reduced relapse rates correlated with expansion of adaptive NK cells, which can be defined by surface expression of the maturation marker CD57 and the activating receptor NKG2C. Adaptive NK cells live longer, are more resistant to immune suppression than canonical NK cells, exhibit properties of immune memory, and their presence in peripheral blood is only observed in CMV seropositive individuals. Given the in vitro and in vivo evidence for enhanced function of adaptive NK cells against malignant cells, we sought to develop a method to preferentially expand this subset in vitro. To this end, we stimulated NK cells isolated from the peripheral blood of healthy CMV seropositive donors for 7 days with IL-15 and either a plate-bound control IgG isotype antibody or an antibody that was determined to be a strong agonist of NKG2C signaling in redirected antibody-dependent cellular cytotoxicity (ADCC) assays. We observed robust proliferation of NKG2C+ NK cells when stimulated with the anti-NKG2C agonist antibody (Figure 1A). High proliferation rates were accompanied by significant induction of the checkpoint inhibitory receptors programmed death-1 (PD-1) and lymphocyte activation gene-3 (LAG-3) (Figure 1B), with LAG-3 expression nearly doubling on NKG2C+ NK cells. LAG-3 is a unique checkpoint inhibitor that ligates MHC class II molecules and is highly expressed on lymphocytes in patients with various types of malignancy.
The stimulated NK cells were also highly active, as evidenced by a complete switch from a CD45RA+CD45RO- to CD45RA-CD45RO+ phenotype (Figure 1C). CD45ROexpression on lymphocytes has been associated with better prognosis in solid tumors including melanoma, lung, and endometrial cancers suggesting a potent ability to target malignant cells.
Despite the increased expression of checkpoint inhibitory receptors, expanded NKG2C+ NK cells remained highly functional. In assays where NK cells were used as effectors against K562 cells, (a myeloid leukemia cell line), we found that NKG2C agonist antibody-expanded NK cells exhibited higher frequencies of tumor necrosis factor (TNF) and interferon (IFN)-γ production compared to NK cells from control IgG isotype cultures. Surprisingly, we found that NK cells expressing LAG-3, instead of exhibiting functional exhaustion, were highly responsive to tumor targets (Figure 1D). To directly test the cytotoxic function of adaptive NK cells expanded with the anti-NKG2C antibody, we analyzed NK cell-mediated killing of dye-labeled K562 cells over the course of 48 hours by live imaging using an IncuCyte Zoom instrument. We observed more rapid killing kinetics and more robust overall target cell killing by adaptive NK cells expanded with the anti-NKG2C agonist antibody relative to the IgG isotype control condition (Figure 1E).
Our data show that CD57+NKG2C+, adaptive NK cells can be efficiently expanded using NKG2C-agonist antibodies. These cells exhibit potent killing abilities and enhanced cytokine secretion, making them ideal candidates for adoptive cell transfer in hematologic malignancies. We also show that LAG-3, a checkpoint inhibitory receptor, is actually associated with enhanced NK cell function in these in vitro assays. This is likely because of the relatively short period of activation (7 days) to which the NK cells are exposed during expansion. There are at least four LAG-3 targeted therapies currently in clinical trials with more in development. A better understanding of the mechanisms of expression of this important receptor and its impact on NK cell function will aid in the rational use of checkpoint inhibitory receptor therapies for cancer patients.
Houchins:Bio-Techne Inc: Employment. Cichocki:Fate Therapeutics Inc.: Consultancy, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.