Introduction
Acute lymphoblastic leukemia (ALL) diagnosed in adolescent and young adults (AYA) poses unique challenges. Despite using more intensive "pediatric-type" protocols, outcomes are generally inferior to those seen in children. The reasons are wide ranging, but when compared to pediatric ALL, AYA ALL has higher-risk biology, poorer tolerance to intensive treatments, and worse compliance with treatment regimens. India has one of the largest AYA populations in the world and AYA-ALL form a significant proportion of leukemias. The Indian acute leukemia research database [INwARD] was established in 2018 and had reported outcomes of ALLs from various centers of all age groups (Korula A, et al. Blood 2018 132:1374). Here, we present data focused on AYA-ALL from this database.
Methods
Retrospective data of AYA (15-29 years) patients with ALL (diagnosed between January 2012 to December 2017) from 9 centers were entered into an independent centralized online data capture system and analyzed for presenting characteristics, treatment and survival outcomes. Protocol choice was based on individual-center preference. For the purpose of this analysis, patients with WBC ≥30000 (B cell) and ≥100,000 (T-cell and other subtypes) were considered as high risk. Intensive protocols (MCP-841, BFM-95, COG), predominantly meant for children were labeled as "pediatric-type" and less intense protocols (GMALL, Hyper CVAD, UKALL) were considered as "adult-type".
Results
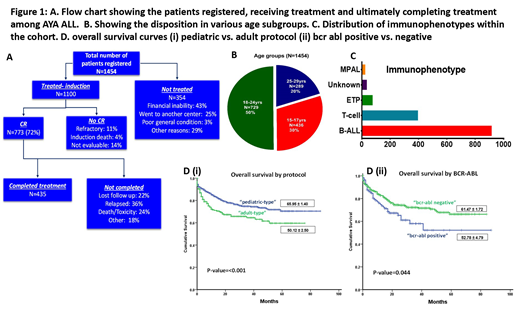
In the 6-year period, 1454 patients were registered [Males: 1114(76%), Median age: 20 years (15-29), Fig. 1.B; Subtype: B -ALL: 916(63%), T-ALL: 396 (27%); Fig. 1.C; High risk disease: 406 (28%)]. Of these,1100 (75%) underwent treatment. Poor financial support was the major reason for not taking treatment (Fig. 1.A).
"Pediatric-type" protocols were used in 881 (81%) patients. After induction, 72% achieved complete remission (CR), 11% were refractory, 4% died during induction and 14% were not evaluable. Minimal residual disease was assessed in 581 and was present in 356 (61%). Attainment of CR, induction mortality, or MRD achievement was not affected by the type of regimen. Among these 1100 patients, 138 (12%) were lost to follow up and did not complete treatment. BCR ABL was tested in 636 and was positive in 112 (17%) [19% among patients with B-ALL (107/557)]and 106 of these were treated with additional tyrosine kinase inhibitors [imatinib (N=83) and dasatinib (N=23)].
Survival analysis: After a median follow up of 21 months, 270 patients relapsed [median time to relapse: 24 months (73% medullary, 17% CNS or testis, and 10% had a combined relapse) and 259 had died. The estimated 2-year event-free (EFS), relapse-free (RFS) and overall survival (OS) were 64%, 75% and 75% respectively. On univariate analysis the factors associated with inferior survival were as follows: EFS: WBC count ≥30,000/cmm, and ECOG PS 2-4; RFS: WBC count ≥30,000/cmm and ECOG PS 2-4; OS: use of "adult-type" protocols, ECOG PS 2-4, and BCR-ABL positive disease. On multivariate cox regression analysis, the only factors associated with inferior OS were: use of "adult" protocols (HR: 1.6), and BCR -ABL positive status (HR1.56) (Fig. 1.D). High WBC count at presentation predicted for inferior RFS while no factor could predict EFS on multivariate analysis.
Conclusions
In a multicenter analysis of AYA-ALL from different parts of India, we found that a quarter of newly diagnosed patients do not start treatment and another 12% are lost from follow up before treatment completion. Majority (80%) of the centers used "pediatric-type" protocols to treat AYA-ALL. Though superior survival was achieved with "pediatric-type" protocols, results must be interpreted with caution as these regimens were likely to be used more often in in younger patients. Variations in treatment protocols used between centers and the retrospective nature of the data are other caveats. Despite these limitations, this is one of the largest reports of AYA ALL from any part of the world and serves as a benchmark for planning prospective studies.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.