Background: Follicular lymphoma (FL) is the most common indolent lymphoma in the western world with a median survival approaching 20 years. However, the course of the disease is extremely heterogeneous and therefore, at diagnosis it is difficult to predict survival. Roughly 20% of patients experience rapid progression of disease post first line treatment. Progression of disease within 24 months of first treatment (POD24) was previously identified a robust predictor of reduced overall survival (OS) (Casulo et al., JCO, 2015).
Aims: We aimed to validate POD24 as a predictor of poor OS in a real-world cohort of patients, which was not uniformly treated, including patients that were initially treated with radiation or observed at least 6 months prior to first line therapy.
Methods: We thoroughly reviewed 635 patient's records that were diagnosed between 1987 and 2018. Patients with FL grade 3B or de-novo transformation, as well as those that were never treated, treated prior to the rituximab era or had missing relevant clinical data were excluded. POD24 was defined as time from first therapy (systemic or radiation therapy) to first documented progression (either clinical or by imaging). Overall Survival was defined as time from diagnosis to either last follow-up or death. Progression Free Survival (PFS) was defined as the time from first treatment to first documented progression, death or last follow-up. Survival was analyzed with Kaplan-Meier method and comparison of survivals was done with Log-Rank test. Multivariate analysis was conducted with Cox regression.
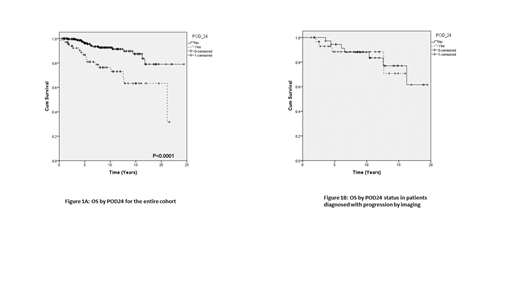
Results: A total of 317 patients met the study inclusion criteria and were included in our analysis. Median age was 57 (23-87), 162 (51%) were male and 155(49%) female .Median follow-up was 7.5 years (0.24-24.4). FLIPI (available in n=149) was high in 41 (27%) patients, intermediate in 37 (25%) and low in 71 (48%). Eighty seven patients (27.4%) received radiation as their first treatment and 86 (27%) were initially observed. Systemic therapy regimens included alkylator based regimens (n=152, RCHOP-88), bendamustine based (45), fludarabine Based (32), and Rituximab alone (2). Maintenance therapy administration was documented in 119 patients. Progression was documented in 133 (42%) patients, and transformation in 34 (11%). Thirty four patients (11%) deceased. Median OS was not reached in our study cohort, and median PFS was 109 months (CI:68-150). Early progression (POD24) was captured in 68 (21.5%) patients. The OS of those patients was significantly lower than those whom did not progress within 24 months of first therapy (figure 1A, p<0.0001). High FLIPI score also predicted lower OS (p=0.001). In multivariate analysis both factors remained significant (POD24 p=0.013, FLIPI p=0.023). In the group of patients that were initially observed (86), 18 had early progression after first treatment. In this group, OS did not differ between the patients that had POD24 vs those who did not (p=0.095). The same was true for patients that had radiation as their first line therapy (p=0.36).
The impact of POD24 on OS was observed in patients that were treated with alkylator based regimens (p=0.02) as well as with bendamustine based regimens (p=0.028). In the Fludarabine treated patients no significant difference in OS was observed in the different POD24 groups, probably due to small sample size. Interestingly, POD24 did not predict inferior OS in 69 patients in whom progression was diagnosed by routine imaging (PET/CT or CT) (Figure 1B). However, it was borderline predictive (p=0.1) when progression was clinically diagnosed (n=38).
Conclusions: Our real-world analysis validated the importance of POD24 as predictor of OS in patients who were treated at diagnosis with alkylator or bendamustine based regimens. POD24 did not predict survival in patients treated with radiation or in those initially observed, a result that may reflect their superior outcome. Notably, POD24 did not predict OS in patients that were diagnosed with progression by routine imaging. As we, and others use imaging studies frequently in the follow-up of FL patients, especially in first two years after therapy, the scenario of positive findings in imaging is relatively frequent. Our data suggest that random findings in imaging that do not have clinical expression may not predict inferior outcome which is of major clinical implications.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.