Introduction
Despite more robust attempts to deliver chemotherapy in the outpatient setting, certain regimens for hematologic malignancies require inpatient hospitalization for treatment and monitoring clinical status. Increased length of stay (LOS) for planned chemotherapy admissions leads to increased healthcare utilization and decreased patient satisfaction. We sought to identify potentially modifiable risk factors for increased LOS.
Methods
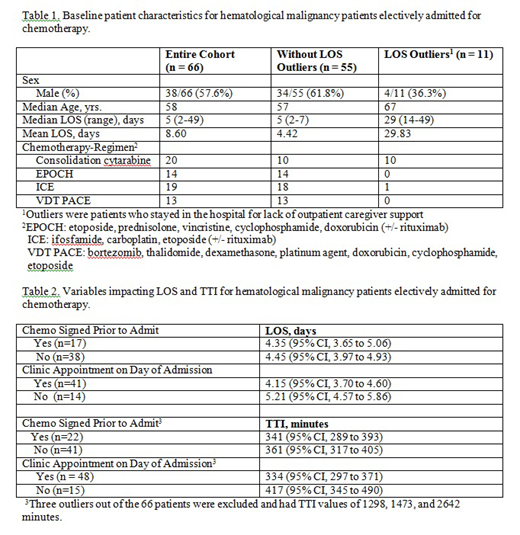
Planned chemotherapy admissions to the inpatient hematology services at Mayo Clinic (Rochester, MN) from October 2018 through March 2019 were reviewed. We included patients who had treatment plans based on four pre-specified common regimens for acute myeloid leukemia, relapsed non-Hodgkins lymphoma and multiple myeloma. Patients who remained in the hospital for lack of caregiver support were excluded. Patient characteristics, including age, malignancy type, and chemotherapy regimen were recorded. Encounter characteristics included day of week of admission, time of admission, time chemotherapy plan initiated, and whether or not all necessary procedures (labs, vascular access, chemo orders) were completed prior to admission. Primary outcome was LOS. Secondary outcome was time to treatment initiation (TTI) after admission.
Results
There were 100 planned admissions for patients receiving four regimens: cytarabine consolidation, EPOCH, ICE, VDT-PACE, during the six month review period. Thirty-six admissions did not occur as planned (regimen changed, rescheduled, or disease progression). Of the remaining 66 admissions, 11 outliers were excluded from primary analysis. Baseline characteristics are summarized in Table 1. Univariate analysis with independent t-test found no difference in LOS for patients who had physician chemotherapy orders in place prior to admission. To the contrary, we detected a non-significant trend toward longer mean length of stay for patients that were not seen in clinic on day of admission (Table 2). On ANOVA, there was a statistically significant difference in LOS when comparing Monday admissions 3.93 days (95% CI 3.07 to 4.79) vs Friday 5.25 days (95% CI, 4.86 to 5.64), but not between any other days. There were no statistically significant differences in TTI when comparing by day of week, physician order status, or chemotherapy regimen. Again, a non-significant trend toward increased TTI was observed for patients not seen in clinic on the same day as admission.
Conclusions
This study serves as a starting point towards identifying modifiable factors that are essential to delivery of safe, satisfying inpatient care to our hematological malignancy patients.Our noteworthy finding regarding patients who were admitted on Friday having a longer LOS than those admitted on Monday requires further exploration. This study is ongoing with mature data to be presented at the meeting.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.