Introduction: The Philadelphia-negative chronic myeloproliferative neoplasms (MPNs) are associated with a high risk of arterial and venous thrombosis, which are attributed to several mechanisms, including elevated blood cell counts per se, in vivo leukocyte and platelet activation with increased adhesion of granulocytes, monocytes and platelets to each other and to a dysfunctional endothelium. In recent years, evidence has accumulated that chronic inflammation is an important pathogenetic mechanism for MPN-disease development and disease progression, inducing increasing genomic instability in hematopoietic cells and thereby emergence of additional mutations of significance for myelofibrotic and leukemic transformation. Recent studies have shown several thrombo-inflammatory genes to be upregulated in patients with MPNs, likely contributing to the increased risk of thrombosis. Several studies have documented that long term treatment with interferon-alpha2 (IFN) is able to normalize elevated cell counts in concert with induction of a remarkable decrease in the JAK2V617F allele burden and accordingly impacting important thrombosis promoting factors in MPNs. Herein, using whole blood gene expression profiling we for the first time report that treatment with IFN is able to normoregulate or significantly downregulate upregulated thrombo-inflammatory genes in patients with MPNs.
Methods: Eight patients with ET, 21 patients with PV, and 4 patients with PMF participated in the study. All patients received treatment with IFN, in the large majority in a dosage ranging from 45-90 ug x 1 sc/week. Gene expression microarray analysis of whole blood was performed before and after 3 months of treatment. Total RNA was purified from whole blood, amplified to biotin-labeled RNA, and hybridized to Affymetrix HG-U133 2.0 Plus chips.
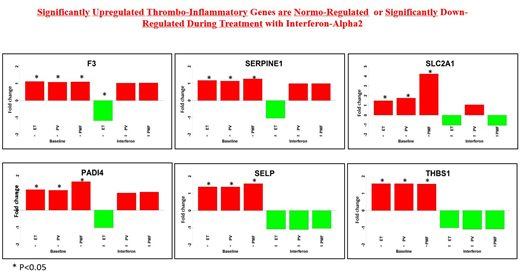
Results: We identified 6261, 10,008, and 2828 probe sets to be significantly differentially expressed in ET, PV, and PMF, respectively, in response to treatment with IFN (pvalue < 0.05). Six thrombo-inflammatory genes were investigated: F3, PADI4, SELP, SERPINE1, SLC2A1, and THBS1. In all patients groups, the 6 genes were significantly upregulated at baseline and either normoregulated or significantly downregulated during treatment with IFN (Figure 1).
Discussion and Conclusions: Thrombosis contributes significantly to morbidity and mortality in MPNs. Despite treatment with conventional drugs (hydroxyurea, anagrelide) - the most used cytoreductive therapies worldwide - patients with MPNs are still suffering potentially life-threatening or life-invalidating thrombotic complications in the brain, heart, lungs and elsewhere. Therefore, there is an urgent need for studies that explore the pathogenetic mechanisms eliciting the thrombotic state and the impact of novel therapies, such as IFN, upon the thrombogenic factors which might be operative. Herein, we have for the first time shown that IFN significantly downregulates several thrombo-inflammatory genes, known to be the upregulated in patients with concurrent or previous thrombosis. Highly intriguing, we found that IFN significantly downregulated the PADI4 gene, which is required for neutrophil extracellular trap (NET) formation and thrombosis development. A most recent study has shown neutrophils from patients with MPNs to be associated with an increase in NET formation, which was blunted by ruxolitinib. This study also showed that JAK2V617F-driven MPN mouse models have a NET-rich, prothrombotic phenotype, highlighting NETosis to be yet another important thrombosis mechanism in MPNs. In conclusion, we have for the first time shown 3 months IFN-treatment to be associated with a significant downregulation of upregulated thrombo-inflammatory genes, including significant downregulation of the NETosis associated gene - PADI4. In the context of a significantly increased risk of thrombosis after the MPN-diagnosis with a particular increased risk at 3 months, our results of significant downregulation of these thrombo-inflammatory genes during IFN-therapy are of paramount importance and may signal an advantage of IFN over conventional cytoreductive therapies. Further studies are required to decipher the impact of IFN upon upregulated thrombo-inflammatory genes and if combination therapy with ruxolitinib may be even more efficacious.
Hasselbalch:Novartis: Research Funding; AOP Orphan Pharmaceuticals: Other: Data monitoring board.
Interferon-alpha for treatment of myeloproliferative neoplasms
Author notes
Asterisk with author names denotes non-ASH members.