INTRODUCTION
Epigenetic alterations are frequent in MDS. EZH2 encodes a histone methyltransferase, which is a catalytic component of polycomb repressive complex 2 crucial for epigenetic silencing of genes involved in stem cell renewal. EZH2 mutation is an independent predictor of overall survival in MDS. Unlike EZH2 Y641 gain-of-function mutation in lymphomas, MDS shows a spectrum of EZH2 mutations without a hotspot that often leads to loss-of-EZH2 function. EZH2 function can also be altered by other mechanisms including mutations in non-coding region, copy number changes and other gene mutations. Assessment of EZH2 protein expression can identify alterations of downstream EZH2 function that may be missed by mutation assessment. In this study, we evaluated EZH2 mutations in MDS patients (pts) and correlated with clinicopathologic findings and outcomes.
METHODS
We searched our institutional database for newly diagnosed MDS pts with EZH2 mutation detected by targeted next-generation-sequencing panels. Consecutive MDS group with wild-type EZH2 served as matched control. EZH2 expression was evaluated by immunohistochemistry (IHC) on decalcified formalin-fixed paraffin embedded bone marrow (BM) biopsies. Nuclear EZH2 staining was independently scored by 3 hematopathologists semi-quantitatively (blinded to data). H-index was obtained by multiplying %positive cells [0, 0%; 1 (1-5%), 2 (6-20%), 3 (21-50%), and 4 (51-100%)] and staining intensity (0-3). H-index of 0-1 was considered negative (MDS-EZH2NONEXP) implying "loss of expression"; ≥2 was considered expressors (MDS-EZH2EXP). Overall survival (OS) was calculated from date of diagnosis to death. Statistical analysis was performed using R version 3.5.1.
RESULTS
We identified 40 (8.8%) MDS pts with 45 EZH2 somatic mutations (35 single; 5 double mutations). There were 33 men and 7 women with a median age of 74 years (range, 55-90). EZH2 mutations included missense (62%), frameshift (27%) and nonsense (11%). Mutations spanned the entire coding region; majority (36%) involved exons 18/19; ~50% were within catalytic SET domain. The median VAF was 31.5 (1.3-92%). EZH2 mutations were frequent within MDS with multilineage dysplasia (16, 40%) and excess blasts (15, 38%) WHO categories. Control group included 38 consecutive MDS pts with wild type EZH2 (MDSEZH2WT).
Twenty-nine EZH2MUTand 37 EZH2WT cases were available for IHC. Assessment in 11 healthy controls (no mutations by targeted NGS panel) showed EZH2 expression in all cases [median score: 9 (range, 6 -12)]. EZH2 expression was lost more frequently in EZH2MUTMDS (69% vs. 26.5%, p=0.001) compared to EZH2WT, majority of which showed preserved staining. Of interest, 9 patients with EZH2WT MDS also showed loss of staining. Hence, we compared outcomes and clinicopathologic features between MDS-EZH2EXP/EZH2NONEXP as well as EZH2MUT/EZH2WT groups.
Compared to EZH2WT, EZH2MUT MDS showed male predominance (54% vs. 83%; p=0.012), frequent chr(7) loss (2.9% vs. 39.3%; p=0.001) and less frequent mutations in splicing factor genes: SF3B1 (37.1% vs. 10%, p=0.006); SRSF2 (25.7% vs. 2.5%, p=0.005); U2AF1 (17.1% vs. 0%) and STAG2 (20% vs. 0%, p=0.003). Compared to MDS-EZH2EXP, MDS-EZH2NONEXP showed frequent chr(7) loss (5.9% vs. 35.7%, p=0.004), less frequent SF3B1 mutation (38.2% vs. 6.9%, p=0.006), lower median platelet count (112 vs. 68, p=0.041) and a trend for higher R-IPSS scores and BM blast%.
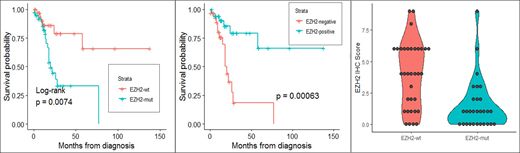
Over the course of the study (median: 14 months), 34 (85%) received hypomethylating agent; 17 (42.5%) died and 12 (30%) patients transformed to acute myeloid leukemia (AML). By univariate analysis, EZH2WT MDS has a significantly better outcome compared to EZH2MUT [not reached (NR) vs. 15 mo, HR 3.39 (1.32-8.73), p=0.011]. MDS-EZH2NONEXP has a significantly better outcome compared to MDS-EZH2EXP (NR vs. 20 mo, HR 0.21 (0.08-0.56), p=0.0017). By multivariate analysis that also included age, gender and R-IPSS, both mutation and protein expression correlated with poor survival, independent of R-IPSS (p=0.027 vs. 0.0063). When mutation and protein expression were analyzed together, protein expression showed a stronger correlation with survival than mutation (p=0.061 vs. p=0.43).
CONCLUSIONS
Both EZH2 mutation and protein loss correlate with poor survival in MDS, independent of R-IPSS. EZH2 protein expression shows a stronger correlation with survival than mutation.
Sasaki:Otsuka: Honoraria; Pfizer: Consultancy. Bueso-Ramos:Incyte: Consultancy. Khoury:Stemline Therapeutics: Research Funding; Angle: Research Funding; Kiromic: Research Funding. Kantarjian:Astex: Research Funding; Daiichi-Sankyo: Research Funding; BMS: Research Funding; Pfizer: Honoraria, Research Funding; Jazz Pharma: Research Funding; Ariad: Research Funding; Actinium: Honoraria, Membership on an entity's Board of Directors or advisory committees; AbbVie: Honoraria, Research Funding; Agios: Honoraria, Research Funding; Cyclacel: Research Funding; Immunogen: Research Funding; Takeda: Honoraria; Novartis: Research Funding; Amgen: Honoraria, Research Funding. Garcia-Manero:Merck: Research Funding; Amphivena: Consultancy, Research Funding; Helsinn: Research Funding; Novartis: Research Funding; AbbVie: Research Funding; Celgene: Consultancy, Research Funding; Astex: Consultancy, Research Funding; Onconova: Research Funding; H3 Biomedicine: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.