Introduction: Venetoclax, a BCL2 inhibitor, has demonstrated efficacy both as a single agent and in combination with rituximabin several subtypes of B-cell non-Hodgkin lymphoma (NHL). The combination of obinutuzumab and lenalidomide has demonstrated safety and preliminary efficacy in follicular lymphoma (Fowler et al., JCO 2015; 35: 7531). We conducted a phase I study of obinutuzumab, venetoclax, and lenalidomide to determine the safety, maximum tolerated dose, and preliminary efficacy of the combination.
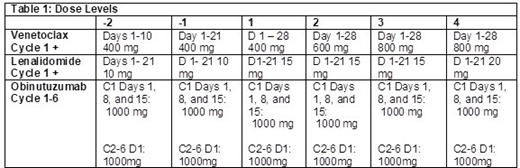
Methods: Patients with relapsed/refractory diffuse large B-cell (DLBCL), transformed, high grade B-cell (HGBCL), marginal zone, and follicular (FL) lymphoma who have received ≥ 1 prior therapy were eligible. Prior autologous (ASCT) but not allogeneic stem cell transplant were permitted. Prior lenalidomide or BCL2 family inhibitors, CNS involvement, and active hepatitis or HIV infection were not permitted. ANC > 1000/mm3, platelets > 75,000/mm3, creatinine clearance ≥50 ml/min, ALT/AST ≤ 3 x ULN, bilirubin ≤ 1.5 x ULN, and ECOG PS 0-2 were required. Treatment consisted of obinutuzumab 1000 mg on days 1, 8 and 15 of cycle 1 and then on day 1 of cycles 2-6 with escalating doses of lenalidomide days 1-21 and venetoclax days 1-28 of a 28 day cycle (Table 1). A 3+3 dose escalation schema was followed. The DLT period was 1 cycle and patients had to receive 80% of the doses of the oral agents and all doses of obinutuzumab to be considered evaluable for DLT. DLTs included: treatment delays > 28 days; ANC < 500 / mm3 or platelets <25, 000 / mm3 persisting > 28 days; grade 4 febrile neutropenia or infection; grade 3 infection that fails to resolve within 7 days; and grade 3 or 4 non-hematologic toxicity. Patients without significant toxicity or progression could continue treatment up to 12 cycles. Response was assessed by CT or PET/CT every 3 months for 12 months and then every 6 months until disease progression.
Results: 22 patients were treated. Median age was 61 years (range 31-78 years) with 16 males. Median prior therapies was 2 (range 1-10) and included 5 patients who had relapsed after chimeric antigen receptor T-cell therapy and 2 patients relapsed after ASCT. Median baseline lactate dehydrogenase was 259.5 U/L (range 147-5133, ULN 190 U/L). 16 patients had aggressive B-cell lymphoma including DLBCL, HGBCL, primary mediastinal and transformed FL, 5 patients had FL and 1 patient had marginal zone lymphoma. At dose level (DL) 1, one patient experienced a DLT, grade 3 neutropenic fever lasting > 7 days. DL 1 was expanded and no additional DLTs occurred. No further DLTs occurred at DL 2-4. DL 4 was expanded and was determined to be the MTD. Four patients, 1 in each dose level, were not evaluable for DLT and were replaced including 3 who did not receiving 80% of the oral agents due to required dose reductions and 1 patient for disease progression. Related grade 3-4 toxicities were primarily hematologic including neutropenia (n=20, 90.9%), thrombocytopenia (n=5, 22.7%), and anemia (n=3, 13.6%). Grade 3-4 infections (n=6, 27%) included sepsis, febrile neutropenia, pneumonia and a urinary tract infection. Other grade 3-4 AEs occurring once each included dysgeusia, dyspnea, nausea, vomiting, and hyperhidrosis. No clinically significant tumor lysis has occurred. Patients have received a median of 3 cycles (range 1-12) of treatment. Three patients remain on therapy and 5 patients are on follow up. Dose reductions of lenalidomide occurred for 17 patients (77%) and of venetoclax for 11 patients (50%). Nine patients have achieved a response (41%), including 8 complete (CR) and 1 partial responses (PR). Responses have occurred at each DL and include 4 patients with FL (2 CR, 2 PR), 4 patients with aggressive lymphoma (4 CR) and 1 patient with MZL (CR). 14 patients are off of the study, 9 with progression, 2 for alternative therapy, and 1 each for DLT, physician preference, and a diagnosis of MDS in a patient with 3 prior lines of chemotherapy.
Conclusions: Combined treatment with obinutuzumab, venetoclax, and lenalidomide administered up to 12 cycles is feasible with activity in multiple subtypes of relapsed NHL. Enrollment in expansion cohorts of FL and aggressive B-cell lymphoma is ongoing.
Christian:Celgene: Research Funding; Janssen: Research Funding; Merck: Research Funding; Seattle Genetics: Membership on an entity's Board of Directors or advisory committees, Research Funding; Cephalon: Research Funding; Bristol-Myers Squibb: Research Funding; Millennium Pharmaceuticals Inc: Research Funding; Genentech: Membership on an entity's Board of Directors or advisory committees, Research Funding; Triphase: Research Funding; Immunomedics: Research Funding; Acerta: Research Funding. Baiocchi:Prelude: Consultancy. Brammer:Verastem, Inc: Research Funding; Viracta Therapeutics, Inc.: Research Funding; Bioniz Therapeutics, Inc.: Research Funding. Epperla:Verastem Oncology: Speakers Bureau; Pharmacyclics: Honoraria. Jaglowski:Juno: Consultancy, Other: advisory board; Kite: Consultancy, Other: advisory board, Research Funding; Unum Therapeutics Inc.: Research Funding; Novartis: Consultancy, Other: advisory board, Research Funding. William:Guidepoint Global: Consultancy; Celgene Corporation: Consultancy; Kyowa Kirin, Inc.: Consultancy; Defined Health: Consultancy; Techspert: Consultancy. Awan:Gilead: Consultancy; AstraZeneca: Consultancy, Speakers Bureau; Abbvie: Consultancy, Speakers Bureau; Pharmacyclics: Consultancy, Research Funding; Sunesis: Consultancy; Janssen: Consultancy; Genentech: Consultancy. Maddocks:BMS: Research Funding; Merck: Research Funding; Pharmacyclics: Membership on an entity's Board of Directors or advisory committees, Research Funding; Novartis: Research Funding; Celgene: Membership on an entity's Board of Directors or advisory committees; Teva: Membership on an entity's Board of Directors or advisory committees.
Obinutuzumab - off label use in relapsed aggressive B-cell lymphoma and indolent B-cell lymphoma Venetoclax - off label use in relapsed B-cell lymphoma
Author notes
Asterisk with author names denotes non-ASH members.