Background: The few established risk factors for non-Hodgkin lymphoma (NHL) exhibit considerable heterogeneity by NHL subtype and suggest an etiologic role for factors with immune- or inflammation-modulating properties, or which otherwise influence lymphocyte proliferation and survival. Epidemiologic evidence supports a potential inverse association for fruit and vegetable intake and NHL risk, but with limited subtype-specific evidence. Glucosinates and indole-3-carbinol, both found in cruciferous vegetables, may mediate tumor suppressive effects, including anti-inflammatory and anti-proliferation effects or restoration of phosphatase and tensin homolog (PTEN), a known tumor suppressor frequently down-regulated in cancer cells. We conducted a prospective study to further elucidate the etiologic role of fruit and vegetable consumption for NHL and its most common histologic subtypes.
Methods: We followed 47,971 men in the Health Professionals Follow-Up Study (HPFS; 1986-2012) and 77,115 women in the Nurses' Health Study (NHS; 1984-2012) with baseline information on diet and no baseline history of cancer. We queried diet every four years using validated food-frequency questionnaires. We calculated fruit and vegetable consumption, in broad categories and for specific food groups, by summing the intake of individual foods excluding fruit juices, potatoes and legumes. Incident NHL diagnoses were first self-reported in study questionnaires then confirmed by review of medical records. We classified histologic subtypes according to the World Health Organization (WHO) and International Lymphoma Epidemiology (InterLymph) Consortium guidelines. We analyzed all NHL (in aggregate) and separate endpoints of chronic lymphocytic leukemia/small lymphocytic lymphoma (CLL/SLL), diffuse large B-cell lymphoma (DLBCL), follicular lymphoma, other B-cell NHL and T-cell NHL. We used multivariate Cox proportional hazards regression adjusting for potential confounding variables to estimate hazard ratios (HR) and 95% confidence intervals (CI) for the association of various fruit and vegetable intake variables with risk of each NHL endpoint. Those intake variables were based on the pre-diagnosis questionnaire returned most recent to NHL diagnosis and modeled as continuous variables in increments of one serving/day.
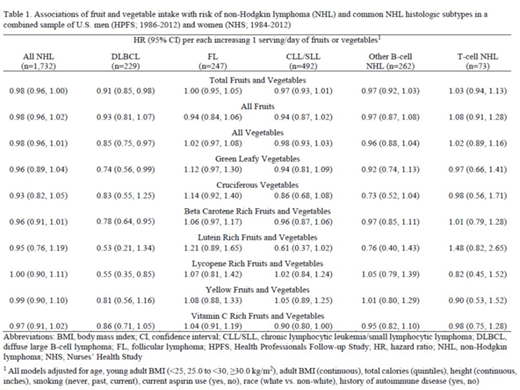
Results: During 2,747,939 person-years of follow-up, we confirmed 1,732 incident NHL cases (986 women, 746 men). In preliminary multivariable-adjusted analyses, no fruit and vegetable intake variable was significantly associated with risk of all NHL (Table 1). Each additional serving/day of all, green leafy, beta carotene rich and lycopene rich vegetables was significantly associated with a 15%-45% lower risk of DLBCL per serving/day but not with other NHL subtypes; cruciferous and lutein rich vegetable intakes had a suggestive but statistically non-significant inverse association with several B-cell NHL subtypes (Table 1). Other associations were only weakly suggestive or null.
Conclusions: In this prospective investigation, preliminary findings suggest a modest reduction of risk of several individual B-cell NHL subtypes, including statistically significantly lower risks of DLBCL, with increasing intake of green and antioxidant rich vegetables. These findings warrant further exploration and confirmation in other study populations. We note that this abstract reports preliminary findings; ongoing analyses will extend the follow-up period, add a third large cohort (NHS II) and assess potential reverse causation, explore sex- and subtype-related heterogeneity and test for non-linearity of observed associations. If confirmed, these results will contribute to evidence-based prevention strategies for NHL and further support general health recommendations concerning benefits of fruit and vegetable intake.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.