Background: Autologous stem cell transplantation (ASCT) can be curative for patients (pts) with relapsed/refractory Hodgkin lymphoma (HL) who are sensitive to salvage therapy, particularly for pts who achieve a complete metabolic response (CMR) before ASCT. Pts who fail multiple salvage regimens have inferior outcomes and are generally considered poor candidates for ASCT. Recent studies suggest that anti-PD-1 monoclonal antibodies (mAbs) may restore sensitivity to cytotoxic therapy in HL pts with previously chemorefractory disease. We hypothesized that PD-(L)1 mAb-based salvage therapy may therefore also improve ASCT outcomes for HL pts who had failed salvage therapy.
Methods: Medical records were reviewed at 13 US transplant centers to identify pts with a diagnosis of classic HL who failed at least 2 systemic therapies, were treated with a PD-1 or PD-L1 mAb (either alone or in combination) as 3rd line or later therapy, and subsequently underwent ASCT.
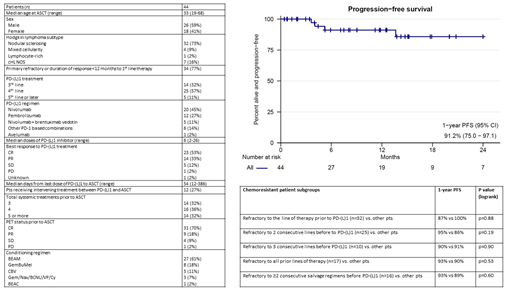
Results: 44 eligible pts were identified. The median age was 33 (range 19-68). Pts received ABVD (39), AVD (2), brentuximab vedotin (BV) + AVD (1), Stanford V (1), or eBEACOPP (1) as 1st line therapy. 26 pts (59%) were refractory to 1st line treatment and 8 additional pts (18%) relapsed within 12 months. High-risk clinical features were observed frequently at 1st relapse including extranodal involvement (47%), B symptoms (27%), and advanced stage (64%). Pts received PD-(L)1 based treatment after failing 2 lines (32%), 3 lines (57%), or ≥4 lines (11%) of therapy. 32 pts (73%) were refractory to the line of therapy before PD-(L)1, 25 pts (57%) to 2 consecutive lines before PD-(L)1, and 10 pts (22%) to 3 consecutive lines before PD-(L)1. 16 pts (36%) were refractory to ≥2 salvage therapies immediately before PD-(L)1 therapy and 17 (39%) were refractory to all prior treatments. 39 pts (89%) received BV or a BV-based combination before ASCT. 67% were BV-refractory, including 86% of those receiving BV monotherapy. Pts received a median of 6 doses of a PD-(L)1 mAb (range 2-26) either as monotherapy (75%) or as part of a PD-1 based combination (25%). The median time from last dose of PD-(L)1 mAb to ASCT was 54 days (range 12-386). Best response to PD-(L)1-based therapy was CR (53%), PR (33%), SD (12%), or PD (2%). The median number of systemic therapies (including PD-(L)1) before ASCT was 4 (range 3-7) and 12 pts (27%) received intervening salvage therapy between PD-(L)1 treatment and ASCT. Pre-ASCT PET status was CR in 31 pts (70%), PR in 9 (18%), SD in 4 (9%), and PD in 1 (2%).
There were no ASCT-related deaths. 2 pts developed BCNU pneumonitis and 1 developed engraftment syndrome. All 3 pts responded to steroids. 14 pts (32%) have received maintenance therapy with BV (4), a PD-1 mAb (8), or BV + PD-1 mAb (2). 4 pts (9%) received consolidative radiation. With a median post-ASCT follow-up of 12.2 months, progression-free survival (PFS) at 1 yr was 91% [95CI 75-97]. Notably, resistance to chemotherapy before PD-(L)1 therapy did not predict worse post-ASCT outcomes (see Table). 1-yr PFS was 90% for pts who were refractory to the 3 lines of therapy before PD-(L)1, 93% for pts refractory to ≥2 salvage therapies immediately before PD-(L)1, and 90% for pts refractory to all prior treatments. Favorable 1-yr PFS was also seen among pts who received PD-(L)1 as 4th or later line therapy (88% vs 100% for pts receiving PD-[L]1 as 3rd line, p=0.17) and among pts who failed to achieve a CMR on pre-ASCT PET (1-yr PFS 81% vs 96% for CMR pts, p=0.34). Lack of response to PD-(L)1 therapy (1-yr PFS 67% vs 96%, p=0.04), receipt of intervening salvage therapy (1-yr PFS 72% vs 100%, p=0.026), and increasing age (HR 1.11, p=0.015) were all significant predictors of inferior PFS. 1-yr overall survival was 100%.
Conclusions: This high-risk cohort is heterogenous in terms of number of prior therapies and degree of chemoresistance, but excellent post-ASCT outcomes were observed among even the most heavily pre-treated, chemorefractory subgroups. Outcomes for PD-(L)1 responders were particularly favorable with a 1-yr PFS of 96%, suggesting that response to PD-(L)1 rather than prior chemotherapy may be the more important predictor of post-ASCT outcomes in this pt population. While longer follow-up is required to confirm the durability of these remissions, ASCT can be considered for HL pts responding to PD-(L)1 based salvage therapy, even if they have previously demonstrated a high degree of chemoresistance.
Nieto:Novartis: Research Funding; Astra-Zeneca: Research Funding; Affimed: Research Funding; Affimed: Consultancy. Byrne:Karyopharm: Research Funding. Maddocks:BMS: Research Funding; Novartis: Research Funding; Teva: Membership on an entity's Board of Directors or advisory committees; Celgene: Membership on an entity's Board of Directors or advisory committees; Pharmacyclics: Membership on an entity's Board of Directors or advisory committees, Research Funding; Merck: Research Funding. Svoboda:BMS: Consultancy, Research Funding; Seattle Genetics: Consultancy, Research Funding; Merck: Research Funding; Incyte: Research Funding; Pharmacyclics: Consultancy, Research Funding; AstraZeneca: Consultancy; Celgene: Research Funding; Kyowa: Consultancy; Kite: Consultancy. McGuirk:Juno Therapeutics: Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding; ArticulateScience LLC: Other: Assistance with manuscript preparation; Pluristem Ltd: Research Funding; Gamida Cell: Research Funding; Kite Pharmaceuticals: Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding, Speakers Bureau; Novartis: Research Funding; Fresenius Biotech: Research Funding; Astellas: Research Funding; Bellicum Pharmaceuticals: Research Funding. Advani:Kyowa Kirin Pharmaceutical Developments, Inc.: Consultancy; Millennium: Research Funding; Janssen: Research Funding; Cell Medica, Ltd: Consultancy; Regeneron: Research Funding; Autolus: Consultancy, Membership on an entity's Board of Directors or advisory committees; AstraZeneca: Consultancy, Membership on an entity's Board of Directors or advisory committees; Stanford University: Employment, Equity Ownership; Agensys: Research Funding; Kura: Research Funding; Pharmacyclics: Consultancy, Membership on an entity's Board of Directors or advisory committees, Research Funding; Roche/Genentech: Consultancy, Membership on an entity's Board of Directors or advisory committees, Research Funding; Bayer: Consultancy, Membership on an entity's Board of Directors or advisory committees; Forty-Seven: Research Funding; Celmed: Consultancy, Membership on an entity's Board of Directors or advisory committees; Bristol-Myers Squibb: Membership on an entity's Board of Directors or advisory committees, Research Funding; Celgene: Research Funding; Takeda: Consultancy, Membership on an entity's Board of Directors or advisory committees; Merck: Research Funding; Seattle Genetics: Consultancy, Research Funding; Infinity Pharma: Research Funding; Gilead Sciences, Inc./Kite Pharma, Inc.: Consultancy, Membership on an entity's Board of Directors or advisory committees. Cohen:Seattle Genetics, Inc.: Consultancy, Research Funding; Bristol-Meyers Squibb Company: Research Funding; Takeda Pharmaceuticals North America, Inc.: Research Funding; Gilead/Kite: Consultancy; LAM Therapeutics: Research Funding; UNUM: Research Funding; Hutchison: Research Funding; Astra Zeneca: Research Funding; ASH: Research Funding; Lymphoma Research Foundation: Research Funding; Genentech, Inc.: Consultancy, Research Funding; Janssen Pharmaceuticals: Consultancy. Frigault:Xenetic: Consultancy; Foundation Medicine: Consultancy; Novartis: Consultancy; Nkarta: Consultancy; Juno/Celgene: Consultancy; Kite/Gilead: Honoraria; Incyte: Consultancy. Chen:Magenta: Consultancy; Takeda: Consultancy; Incyte: Consultancy; Kiadis: Consultancy; Abbvie: Consultancy. Lynch:Johnson Graffe Keay Moniz & Wick LLP: Consultancy; Rhizen Pharmaceuticals S.A: Research Funding; Juno Therapeutics: Research Funding; Takeda Pharmaceuticals: Research Funding; Incyte Corporation: Research Funding; T.G. Therapeutics: Research Funding. Smith:Seattle Genetics: Research Funding; Denovo Biopharma: Research Funding; Ayala (spouse): Research Funding; Merck Sharp & Dohme Corp: Consultancy, Research Funding; Acerta Pharma BV: Research Funding; Incyte Corporation: Research Funding; Ignyta (spouse): Research Funding; Genentech: Research Funding; Bristol-Myers Squibb (spouse): Research Funding; Portola Pharmaceuticals: Research Funding; Pharmacyclics: Research Funding; AstraZeneca: Membership on an entity's Board of Directors or advisory committees, Research Funding. Ho:Jazz Pharmaceuticals: Research Funding; Jazz Pharmaceuticals: Consultancy; Omeros Corporation: Membership on an entity's Board of Directors or advisory committees. Armand:Affimed: Consultancy, Membership on an entity's Board of Directors or advisory committees, Research Funding; Bristol-Myers Squibb: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding; Merck: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding, Speakers Bureau; Sigma Tau: Research Funding; Infinity: Consultancy; Otsuka: Research Funding; Genentech: Research Funding; Pfizer: Consultancy; ADC Therapeutics: Consultancy; Tensha: Research Funding; Roche: Research Funding; Adaptive: Consultancy, Membership on an entity's Board of Directors or advisory committees, Research Funding. Herrera:Merck: Consultancy; BMS: Consultancy; Genentech: Research Funding; Adaptive Biotechnologies: Consultancy; Gilead Sciences: Research Funding; KiTE/Gilead: Consultancy; Genentech: Consultancy; Merck: Research Funding; Astra-Zeneca: Research Funding; Seattle Genetics: Consultancy; BMS: Research Funding; Seattle Genetics: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.