INTRODUCTION
Sepsis is a life-threatening organ dysfunction caused by dysregulated host response to infection. Early detection of sepsis is very crucial in its management, as there is an increase of 8% mortality for every hour delay in commencing therapy (Kumar et al., 2006). A wide variety of diagnostic techniques proposed, could not be clinically translated due to poor sensitivity & specificity, high levels of heterogeneity and complexity of assay preparation. Currently most clinical settings depend on Procalcitonin (PCT) and C-reactive protein (CRP) for diagnosis, which also lack sensitivity and specificity.
The objective of our study was early detection of sepsis in patients undergoing cardiac surgery. Blood stream infection, confirmed by blood culture (the gold standard), requires large turnaround time and is less sensitive here due to prophylactic antibiotics. SOFA score overestimate the probability of sepsis due to the impaired cardiovascular parameters and inotrope support (Howitt et al., 2018). The Society of Thoracic Surgeons (STS) criteria to detect sepsis need positive blood culture to identify sepsis within the first 48 hours post-surgery. Since none of the above can cater early diagnosis, the most appropriate way is to target dysregulated host response. It has been reported that increased expression of CD64, on neutrophil surface (nCD64) is associated with proinflammatory response and down-regulation of HLA-DR expression on circulating monocytes (mHLA-DR) is associated with anti-inflammatory response in humans. Citing this interplay between pro and anti-inflammatory response in sepsis, we hypothesized that the relative expression of these antigens may detect dysregulated host immune response and thereby may provide a criterion for early diagnosis of sepsis
MATERIALS AND METHODS
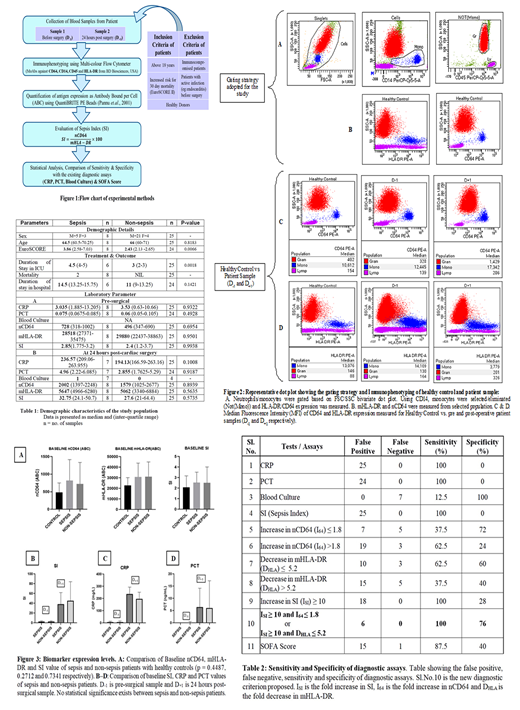
A flowchart of the experimental steps is shown in Fig1. Adult patients, who underwent cardiac surgery, were selected for this double-blinded study after the approval from the appropriate Institutional Ethics Committee. The study was un-blinded after the initial set of experiments, with biochemical and clinical outcome of the patients. The data sets were analyzed (GraphPad Prism v8.1.1) and a p value of < 0.05 was considered statistically significant
RESULTS
Out of the total patients (n=33), 7 patients were diagnosed with suspected sepsis and 1 with proven sepsis as per STS criteria, substantiated by longer ICU and hospital stay (Table1). The optimized Flowcytometry panel and gating strategies is shown in Fig.2
The expression of nCD64, mHLA-DR and SI (Sepsis Index) in all patients before surgery did not show any statistically significant difference with that of healthy controls [Figure-3A]. At 24 hours post-surgery, all patients had significant up-regulation of nCD64 and down-regulation of mHLA-DR. A similar significant elevation was observed in CRP and PCT [Figure-3 B-D], but insignificant difference exists between sepsis and non-sepsis patients (p values in Table1). Therefore the diagnostic efficacy of all this measurements and scoring scheme, in identifying sepsis at 24 hours was poor (Table2)
A useful diagnostic criterion is obtained by calculating the fold increase in nCD64 (I64) & SI (ISI) and fold decrease in mHLA-DR (DHLA) at 24 hour. It was observed that many patients had ISI≥10, due to I64 approximately 2 and DHLA 5. Based on this observation, a diagnostic criterion able to detect 'dysregulated host immune response' at 24 hour post-surgery is identified. The criterion is: 10 fold or more increase in SI combined with either ≤1.8 fold increase in nCD64 or ≤5.2 fold decrease in mHLA-DR.
CONCLUSION
The data obtained from this pilot study was analysed based on different criteria to identify the best possible way to detect the onset of sepsis post-cardiac surgery. The discriminative power of many tests to differentiate sepsis and SIRS is inadequate. We propose a combination of fold changes in antigen expression, which could so far, identify all sepsis patients, since the measurements detect the underlying biological mechanism, picking up both exacerbated proinflammatory response and immunoparalysis. The significance of the result is that the proposed diagnostic criteria could potentially pre-empt diagnosis of sepsis at 24 hours post-surgery, before the onset of any clinically identifiable symptoms of the disease. This needs to be substantiated by extending the study on a larger patient cohort.
Mony:BD Biosciences: Research Funding. Jain:BD Biosciences: Employment.
Author notes
Asterisk with author names denotes non-ASH members.