BACKGROUD: HyperCVAD is one of the most frequent used protocols in adult ALL in routine practice. On the other hand, the CALLG2008 protocol was a published protocol designed by the Chinese Acute Lymphoblastic Leukemia Cooperative Group for adult ALL. In this retrospective study, we analyzed 70 Chinese patients with adult ALL to compare the efficacy, safety and costs of HyperCVAD regimen in comparison to CALLG2008.
METHODS: Pts ≥ 15 years old with previously untreated newly-diagnosed ALL were eligible. All pts provided IRB-approved informed consent before chemotherapy. HyperCVAD and CALLG2008 were given as initially described. Imatinib (400 mg daily) was administered concurrently in patients with Ph-positive ALL. Prophylactic antibiotics, antifungals, and antiviral agents were provided according to the institutional guidelines. Red blood cells and platelet transfusions were given for hemoglobin<60 g/L and platelets≤10×109/L or if with hemorrhage. Granulocyte colony-stimulating factor was given routinely. Bone marrow aspiration was performed after the completion of the first course of induction chemotherapy to assess their response to treatment. All patients were evaluated for minimal residual disease (MRD) in bone marrow at the end of the first course of induction by 6-color multi-parametric flow cytometry analysis and reverse-transcription quantitative polymerase chain reaction (RT-qPCR).
Primary endpoint of the study was CR rate after the first course of induction therapy. Complete remission (CR) was defined as having <5% marrow blasts, a normalization of peripheral counts (neutrophil count ≥1 × 109/L, platelet count ≥100 × 109/L, and no abnormal peripheral blasts), and absence of extramedullary disease. The criteria for the positive and negative MRD are based on the experience of the European ALL MRD Detection Research Collaborative Group. Adverse events occurring during the first 8 weeks after the first course of induction therapy are reported. Other treatment outcomes including blood transfusion requirement, recovery day of neutrophil count were collected, as well as detailed data regarding hospitalization time, complications and costs.
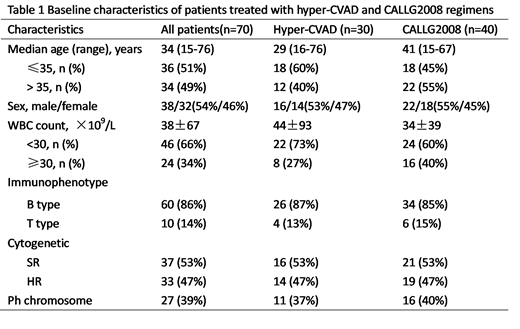
RESULTS: Thirty patients were treated with HyperCVAD, and 40 with CALLG2008. Pre-treatment characteristics are shown in the Table 1. After the first course of induction chemotherapy, complete remission was obtained in 83% and 78% of patients, respectively. The CR rate did not vary significantly by different regimens, gender, age, immunophenotype. However, 96% of those with cytogenetic or molecular evidence of the Philadelphia (Ph) chromosome and 76% of those without such evidence achieved a CR (P=0.045). In Ph-negative group, MRD-negative rates were found to be significantly higher with HyperCVAD (58% vs 27%, P=0.036). The median durations of neutrophil recovery of CALLG2008 group was 4 days longer than HyperCVAD group (P=0.038). Moreover, grade 3-4 thrombocytopenic (<500/μl) was more frequent on CALLG2008 regimens compared with the HyperCVAD regimens (90% vs 63%; P=0.007). Accordingly, a lower platelet transfusion rate was observed in favor of the HyperCVAD group (47% vs 73%, P=0.007). The CALLG2008 regimen had more all-grade hepatic toxicity than HyperCVAD regimen (53% vs 27%; P=0.03). Grade 3-4 hypofibrinogenemia was more frequent on CALLG2008 regimen compared with hyper-CVAD regimen (33% vs 7%; P=0.009). The average time to stay of the first course of chemotherapy were 19.4±3.5 and 24.2±8.6 days in HyperCVAD and CALLG2008 groups, respectively (P=0.002). The average drug-related costs for patients treated with HyperCVAD were significantly lower compared with that for those treated with CALLG2008 (30981.7 vs 59422.9 yuan, P=0.010).
CONCLUSION: Although HyperCVAD and CALLG2008 regimens showed relatively similar early CR rate, the former yields deep remissions more powerfully in Ph-negative ALL. Additionally, HyperCVAD was more favorable in hematopoietic recovery than CALLG2008. Differences were also observed in terms of less complications, shorter hospitalization and lower drug-related expenditure in favor of HyperCVAD group.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.