Background:
Previous studies show that the use of single-unit unrelated cord blood transplantation (sUCBT) for severe aplastic anemia (SAA) has poor outcome because of high incidence of primary graft failure. Effective measures to completely prevent rejection in SAA remain to be identified, but higher cell dose, less HLA disparities and better conditioning regimen are known to improve the outcome. In this study we compare two conditioning regimens to determine which is better to facilitate engraftment after sUCBT.
Patients and methods:
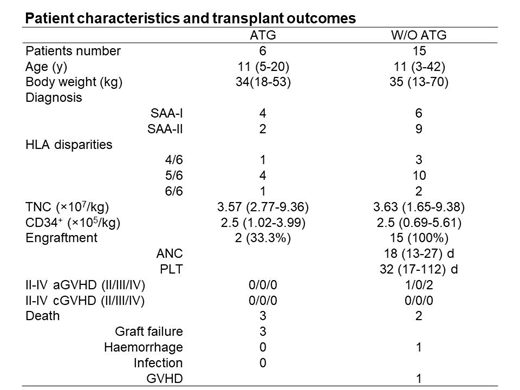
We retrospectively analyzed the outcomes of 21 Chinese patients with acquired SAA who do not have HLA-matched siblings and do not respond to first-line immunosuppressive therapy with ciclosporin (CSA) and/or anti-thymocyte globulin (ATG) that received sUCBT were included beteween July 2016 and October 2018. Data collected as of June 2019 were analyzed. 6 patients (ATG group) used a conditioning regimen consisting of ATG (rabbit) 2.5 mg/kg (D-9 to D-7) with fludarabine 30 mg/m2 (D-9 to D-4), cyclophosphamide 60 mg/kg (D-3 to D-2) and total body irradiation (3 Gray) on D-1. Median age at time of sUCBT was 11 (5-20) years, median body weight was 34(18-53)kg. Waiting time from diagnosis to transplantation was 427(277-3407)days. The median total nucleated cell number and CD34-positive cell number at infusion were 3.57(2.77-9.36) × 107/kg and 2.5(1.02-3.99) × 105/kg, respectively. Another group (No-ATG) of 15 patients used a conditioning regimen without ATG consisting of fludarabine 40 mg/m2 (D-8 to D-4), cyclophosphamide 60 mg/kg (D-3 to D-2) and total body irradiation (4 Gray) on D-1. Median age at time of UCBT was 11 (3-42) years, median body weight was 35(13-70)kg. Waiting time from diagnosis to transplantation was 1664(160-2006)days. The median total nucleated cell number and CD34-positive cell number at infusion were 3.63(1.65-9.38)×107/kg and 2.5(0.69-5.61)×105/kg, respectively. CsA and MMF was given to both groups as prophylaxis for graft versus host disease (GVHD).
Results:
Primary graft failure was observed in 4 out of 6 patients in ATG group. All of these 4 patients received salvage transplantation with haploidentical related donor, 3 patients died after salvage transplantation due to grade IV GVHD in intestinal tract and infection. However, all of 15 patients in the No-ATG group had completely engraftment. The median time to neutrophil engraftment was 18 (13-27) days, platelet engraftment was 32 (17-112) days. 42-day cumulative incidence of engraftment is 100% compared to 33% in ATG group (P=0.008). During follow-up, 2 patients died before 1 year due to renal failure (n=1) and encephalorrhagia (n=1) in the No-ATG group. One-year survival rate is 86.7% in No-ATG group compared to 50% in ATG group (P=0.0598).
Conclusion:
sUCBT after a FLU-CY-TBI conditioning regimen was an effective and safe option for SAA patients, with better engraftment and survival. Pediatric and adult SAA patients who are younger than 50 years old, lack of HLA-matched sibling donor and refractory to immunosuppressive therapy should consider sUCBT.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.